Post-COVID Stress Disorder: Another Emerging Consequence of the Global Pandemic
The pandemic has triggered an array of emotional, physical, and economic issues but in the midst of this crisis, nations have shared and learned from each other’s experiences.
kalafoto/AdobeStock

Throughout 12,000 years of human history, pandemics have killed an estimated 300 million to 500 million people, with the bubonic plague decimating an estimated 60% of the European population during the Middle Ages. Despite modern advances in medicine, coronavirus disease 2019 (COVID-19) has caused more than 1 million reported deaths in less than a year. Aside from the death toll, the pandemic has triggered significant emotional, physical, and economic problems around the world. But even in the midst of this crisis, nations have an opportunity to share and learn from each other’s experiences.
The emerging literature measures the impact of various traumatic stressors related to COVID-19, as well as the effects of less severe types of stress exposures. COVID-19 has already led to diverse mental health problems, including anxiety, depression, posttraumatic stress disorder, and other trauma- and stress-related disorders. Different groups have met the qualifying criteria for posttraumatic stress disorder (PTSD) according to DSM-5 as a result of the pandemic: those who have themselves suffered from serious COVID-19 illness and potential death; individuals who, as family members and health care workers, have witnessed others’ suffering and death; individuals who have learned about the death or risk of death of a family member or friend due to the virus; and individuals who have experienced extreme exposure to aversive details (eg, journalists, first responders, medical examiners, and hospital personnel).
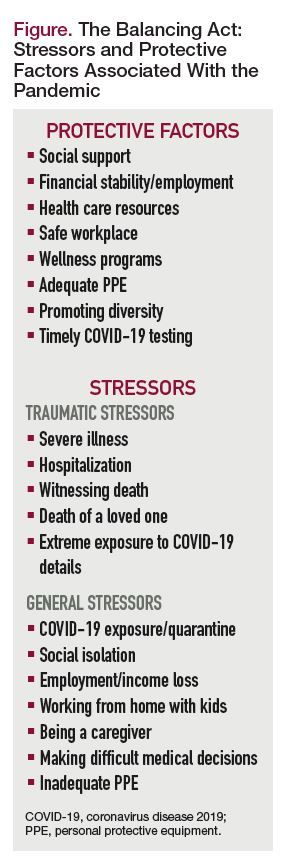
Moreover, studies have explored other stressors adding to individuals’ emotional burdens, such as social isolation, unemployment and economic losses, and working from home while caring for children and other family members. Among health care workers, strains include lack of personal protective equipment (PPE), fears of virus exposure, burnout, patients perishing despite heroic efforts to save them, and difficult decisions about which patients should receive limited resources. A few studies have examined posttraumatic stress symptoms (PTSS), as well as anxiety, depression and other symptoms, and substance use in the general population during the pandemic.
More time is needed, of course, to conduct and publish systematic investigations on mental health sequelae, such as formal psychiatric diagnoses. Studies generally have been conducted through diverse internet platforms, which may affect generalizability. Methods and validated rating scales vary.
At the same time, it is not too soon for clinicians to read the emerging literature and base treatments on the latest research. We will explore some representative international studies of various groups affected by COVID-19, as well as protective factors and suggested interventions to help those in need (Figure).
Highly Exposed Individuals
Much of the current research emerges from China, the first country confronted by the pandemic. A study of nurses in China exposed to COVID-19 found a PTSD incidence of 16.8%, with highest scores in avoidance symptoms.1 Job satisfaction was associated with lower PTSD symptom scores and positive coping. The authors recommended supporting nurses who are having difficulty coping with their work by providing counseling.
A web-based, cross-sectional survey of more than 7000 Chinese individuals in February 2020 found that health care workers had the highest rate of poor sleep, and those aged 35 years or younger had more mood and anxiety symptoms.2 Overall, 35.1% of respondents reported anxiety symptoms, 20.0% depressive symptoms, and 18.2% poor sleep quality.
Other international studies have examined stress responses in health care workers treating patients with COVID-19. A study of 900 health professionals caring for hospitalized patients with COVID-19 in Singapore and India found relatively low symptoms of anxiety (15.7%), depression (10.6%), and stress (5.2%).3 However, among health care workers reporting these issues, more than half had symptoms in the moderate to extremely severe range. In addition, 67% of respondents reported physical symptoms, especially headache, lethargy, anxiety, and insomnia, suggesting somatic expressions of distress. United Kingdom military health care workers were assessed for the effects of inadequate safety equipment on their mental health during the COVID-19 medical response. Those with inadequate equipment had greater odds of having common mental health disorders (2.49), PTSD (2.99), poorer global health (2.09), and emotional problems (1.69).4
Only a few studies of mental health problems among patients hospitalized with COVID-19 have been published, with more to come. A study of hospitalized but stable patients found a high prevalence of PTSS (96.2%).5 A chart review of hospitalized patients with COVID-19 in Spain found more than half of the 841 patients hospitalized with COVID-19 had a neurological symptom. Of these, nonspecific neurological symptoms were identified, as well as disorders of consciousness (19.6%), mostly in elderly patients and in those with severe COVID-19 disease; myopathy (3.1%); dysautonomia (2.5%); and other less frequent symptoms.6 Neuropsychiatric symptoms were reported by 19.9% of these patients, including insomnia, anxiety, depression and psychosis; these were not associated with disease severity.6
Some studies have drawn inferences based on other severe respiratory viruses. A meta-analysis of long-term clinical outcomes for survivors of adult severe acute respiratory syndrome (SARS) and Middle East Respiratory Syndrome (MERS) who were in the intensive care unit (ICU) revealed PTSD prevalence in 39%, depression in 33%, and anxiety in 30% beyond 6 months after discharge, as well as reduced lung function and reduced exercise capacity.7 Italian experts also concluded that we might anticipate similar outcomes in survivors of COVID-19.8
Acute respiratory distress syndrome (ARDS) in ICU survivors of COVID-19 may occur, with an expected survival rate of approximately 25%. Survivors of ARDS may experience persistent fatigue and poor exercise tolerance, pain and weakness, neurological sequelae, and the psychological effects of prolonged ICU stays, as noted in patients with MERS and SARS. Stressors included immobility, separation from family and friends, prolonged sedation, anxiety about health conditions and survival, and subsequent job loss. The authors emphasized the need to identify PTSD (anticipated in up to 30% of ARDS survivors) and other mental health problems, and to provide appropriate and timely multidisciplinary therapy that should continue after discharge.8 A literature review of studies linking panic disorder with patients who had SARS suggested that aggravation of panic attacks is highly likely in survivors of COVID-19 in the face of prominent respiratory symptoms, as panic may be triggered by fear conditioning to abnormal breathing problems.9 The authors urged monitoring for panic as well as obsessive compulsive disorder, PTSD, and generalized anxiety disorder.
Exposure to Nontraumatic Stress
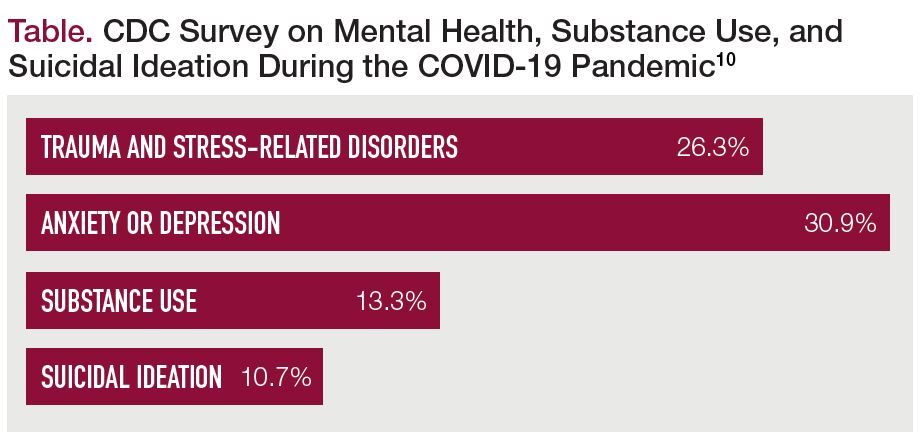
Some mental health care advocates believe the general population may be suffering from various levels of vicarious traumatization, although strictly speaking this would not qualify for PTSD’s Criterion A for trauma exposure. Along these lines, in August 2020 the CDC published results of a large US web-based survey of more than 5000 adults (Table),10 in which 40.9% endorsed at least 1 adverse mental or behavioral health problem related to the pandemic. Symptoms of a trauma- and stressor-related disorder were reported by 26.3%, symptoms of anxiety or depression by 30.9%, substance use to cope by 13.3%, and serious consideration of suicide in the prior days by 10.7%. Suicidal ideation was significantly higher for younger respondents aged 18 to 24 years (25.5%), minority groups (Hispanic individuals, 18.6%; Black individuals, 15.1%), nonpaid caregivers for adults (30.7%), and essential workers (21.7%). The authors stressed the need to identify at-risk individuals to develop policies to address health inequities, and to increase resources for identifying mental health problems and offering new treatment options, including telehealth treatments.10
Table. CDC Survey on Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic10
In a study of home-quarantined youth in China during the first month of the COVID-19 outbreak, 12.8% had PTSS levels consistent with PTSD, with PTSS and distress associated with negative coping styles.11 Symptom levels were expected to increase with time as quarantine continued. This is important since a formal diagnosis of PTSD requires symptoms to persist for more than a month.
In another online survey conducted early during the Wuhan outbreak, researchers looked at anxiety and depression symptoms (rather than specific PTSS) in relation to social media exposure (SME) to COVID-19 news. The study, which included approximately 5000 adults in China, found high SME was positively associated with higher odds of anxiety and a combination of depression and anxiety, compared with low SME.12 A longitudinal survey of the general population in China during the initial outbreak, and again 4 weeks later, found the mean Impact of Events Scores to be above the cutoff scores for PTSD symptoms at both times, with moderate to severe stress, anxiety, and depression levels.13
Results of an Italian cross-sectional, web-based survey showed a relatively high percentage (29.5%) of PTSS related to the pandemic, suggesting that the pandemic itself could be considered a traumatic event.14 Similarly, an online survey of almost 3500 people in Spain found symptoms of PTSD (15.8%), depression (18.7%), and anxiety (21.6%), with loneliness the strongest predictor of symptoms.15 Other factors associated with these problems were female gender, previous mental health or neurological problems, having physical symptoms similar to those of COVID-19, or having a close relative infected.
Nursing home residents have been particularly vulnerable to poor health outcomes; early in the COVID-19 pandemic many facilities adopted strict lockdown policies. However, social isolation is particularly detrimental to the elderly, who may have increased risk for depression, anxiety, worsening dementia, and even earlier death.16 Given these issues, the Centers for Medicare and Medicaid Services (CMS) recommended safe communal activities for locked-down nursing homes.
In Canada, researchers explored prenatal maternal distress before and during the COVID-19 pandemic.17 Women assessed during the pandemic had higher levels of depression and anxiety, with levels more likely to be clinically significant, compared with women assessed before COVID-19. During the pandemic, dissociative and PTSD symptoms and negative affectivity were also greater, underscoring the need to carefully assess pregnant women to help prevent negative, stress-related outcomes in mothers and infants.
Perhaps not surprisingly, when compared with a control population, psychiatric inpatients in China had more PTSD, anxiety, and depression symptoms; more anger, impulsivity, and worries about health; and intense suicidal ideation.18 Hospitalized psychiatric patients and their mental health caregivers are at high risk for COVID-19 infection, compounding their existing stress. This was noted early in February 2020 in Wuhan, when the virus was diagnosed in at least 50 inpatients with psychiatric disorders and 30 mental health professionals. Factors included lack of protective gear and difficulties isolating.19 Outpatients with psychiatric disorders are also vulnerable to emotional distress during a pandemic. An online survey of more than 2000 outpatients in China discovered that 20.9% of patients with preexisting psychiatric disorders had seen their symptoms get worse during the pandemic.20
Interventions
How can we help individuals whose mental health has been harmed by COVID-19?
To support medical caregivers assigned to the front line during the pandemic, experts advise addressing burnout, as prolonged problems may overlap and lead to acute stress disorder and PTSD.21 Suggestions have ranged from practical measures (such as ensuring adequate PPE, handwashing, and decontamination of surfaces) to developing personnel policies that reassign at-risk medical personnel away from high-risk sites, ensure the safety of their family members, and stress the importance of self-care.22 Also recommended is providing health care workers access to child care services during expanded work hours and school closures. Workers should have adequate rest and breaks, be excused from less-essential tasks, and have regular information and feedback sessions with managers and the community. In many areas, hospitals provide telephone hotline teams trained to provide psychological assistance. Professional organizations offer physician wellness programs to provide free, confidential sessions to deal with burnout, adjustment problems, family issues, and other mental health sequelae.
The increasing numbers of people who were seriously ill with COVID-19 should be assessed for physical symptoms of chronic pain,8 with physical therapy and medications adjusted to avoid opioid dependence. Survivors of ARDS should receive evidence-based medications, cognitive behavioral therapy, and other psychotherapies for PTSD, panic, depression, and other mental disorders.
To combat isolation among locked-down nursing home residents, CMS recommends safe communal activities such as book clubs, movies, bingo, and outdoor family visits (ie, on lawns or in parking lots) with precautions of social distancing and PPE. Some nursing homes have provided live music, parades, therapy animals, recordings and photos of loved ones, physical contact with loved ones through plastic protective barriers, and even physical and occupational therapy sessions held outdoors.16
Psychological first aid provided by trained community personnel might help the general population as they experience distress during the COVID-19 pandemic.2 For individuals enduring fallout from personal stressors, experts have recommended expanded use of telehealth to identify and treat mental health conditions, including depression, PTSD and other trauma-related disorders, substance use disorders, and suicidal ideation. Self-help groups, 12-step programs, spiritual and religious services, interest groups, and employee groups working from home are all increasingly using interactive internet-based platforms. And it is essential for societies to provide citizens with assistance for jobs, housing, food, medical care, education, internet connections, and many other basic survival needs.
The current international pandemic and possibly future ones will challenge us and give us the chance to continue to learn and share with other nations, hopefully linking us cooperatively rather than polarizing us.
Phebe Tucker, MD is professor and vice chair of education, Department of Psychiatry, University of Oklahoma Health Sciences Center, Oklahoma City. Christopher Czapla, MD is assistant professor and residency training director, Department of Psychiatry, University of Oklahoma Health Sciences Center, Oklahoma City. Authors have no relevant financial conflicts of interest. This article was originally posted on October 5, 2020, and has since been updated.
References
1. Wang YX, Guo HT, Du XW, et al. Factors associated with post-traumatic stress disorder of nurses exposed to corona virus disease 2019 in China. Medicine (Baltimore). 2020;99(26):e20965.
2. Huang Y, Zhao N. Mental health burden for the public affected by the COVID-19 outbreak in China: Who will be the high-risk group? Psychol Health Med. 2020;1-12.
3. Chew NWS, Lee GKH, Tan BYQ, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. 2020;88:559-565.
4. Simms A, Fear NT, Greenberg N. The impact of having inadequate safety equipment on mental health. Occupational Medicine. 2020;70(4):278-281.
5. Bo HX, Li W, Yang Y, et al. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol Med. 2020;27:1-2.
6. Romero-Sánchez CM, Díaz-Maroto I, Fernández-Díaz E, et al. Neurologic manifestations in hospitalized patients with COVID-19: The ALBACOVID registry. Neurology. 2020;95(8):e1060-e1070.
7. Ahmed H, Patel K, Greenwood DC, et al. Long-term clinical outcomes in survivors of severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus outbreaks after hospitalization or ICU admission: A systematic review and meta-analysis. J Rehabil Med. 2020;52(5):jrm00053.
8. Vittori A, Lerman J, Cascella M, et al. COVID-19 Pandemic acute respiratory distress syndrome survivors: pain after the storm? Anesth Analg. 2020 Jul;131(1):117-119.
9. Javelot H, Weiner L. Panique et pandémie: revue de la littérature sur les liens entre le trouble panique et l’épidémie à SARS-CoV-2 [Panic and pandemic: Review of the literature on the links between panic disorder and the SARS-CoV-2 epidemic]. Encephale. 2020 Jun;46(3S):S93-S98.
10. Czeisler MÉ , Lane RI, Petrosky E, et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic — United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1049–1057.
11. Liang L, Gao T, Ren H et al. Post-traumatic stress disorder and psychological distress in Chinese youths following the COVID-19 emergency. J Health Psychol. 2020;25(9):1164-1175.
12. Gao J, Zheng P, Jia Y et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. 2020;15(4):e0231924.
13. Wang C, Pan R, Wan X, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. 2020;87:40-48.
14. Forte G, Favieri F, Tambelli R, Casagrande M. COVID-19 Pandemic in the Italian Population: Validation of a Post-Traumatic Stress Disorder Questionnaire and Prevalence of PTSD Symptomatology. Int J Environ Res Public Health. 2020;17(11):4151.
15. González-Sanguino C, Ausín B, Castellanos MÁ, et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun. 2020;87:172-176..
16. Abbasi J. Social isolation—the other COVID-19 threat in nursing homes. JAMA. 2020;324(7):619-620.
17. Berthelot N, Lemieux R, Garon‐Bissonnette J, et al. Uptrend in distress and psychiatric symptomatology in pregnant women during the coronavirus disease 2019 pandemic. Acta Obstet Gynecol Scand. 2020; 99: 848– 855.
18. Hao F, Tan W, Jiang L, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun. 2020;87:100-106.19. Xiang YT, Zhao YJ, Liu ZH, et al. The COVID-19 outbreak and psychiatric hospitals in China: managing challenges through mental health service reform. Int J Biol Sci. 2020;16(10):1741-1744. Published 2020 Mar 15.
20. Zhou J, Liu L, Xue P, et al. Mental Health Response to the COVID-19 Outbreak in China. Am J Psychiatry. 2020;177(7):574-575.
21. Restauri N, Sheridan AD. Burnout and Posttraumatic Stress Disorder in the Coronavirus Disease 2019 (COVID-19) Pandemic: Intersection, Impact, and Interventions. J Am Coll Radiol. 2020;17(7):921-926.
22. Adams JG, Walls RM. Supporting the Health Care Workforce During the COVID-19 Global Epidemic. JAMA. 2020 ;323(15):1439-1440.