4 common myths about Narcan, the ‘antidote’ to opioid overdose
The FDA-approved nasal spray can even be used on and by children.
When it comes to tackling the opioid crisis in America, there is no single solution. Public health officials have taken measures to prevent future overdoses by reducing the number of opioid prescriptions, curbing the flow of illicit drug trafficking, and raising awareness of the dangers of opioids. But for the three million people already addicted to this class of drugs, the emphasis has turned to a quick-working treatment: naloxone.
It’s possible to reverse an opioid overdose with an injectable or single-dose nasal spray called naloxone (also known by the brand name Narcan). Street drugs and prescription painkillers like heroin, morphine, and codeine target opioid receptors in the brain to induce a pleasurable high. But they can also affect neurons that control respiration, causing a person to stop breathing if they overdose. Naloxone blocks the brain receptors so that the drugs can’t reach them, preventing this deadly side effect. “There are very few things I would call a perfect antidote, but, in this case, Narcan is one of them,” says Ryan Marino, a medical toxicologist and addiction medicine specialist at the Case Western Reserve University School of Medicine. He adds that naloxone works against synthetic opioids like fentanyl.
[Related: At-home test strips for fentanyl are just the first step to preventing overdoses]
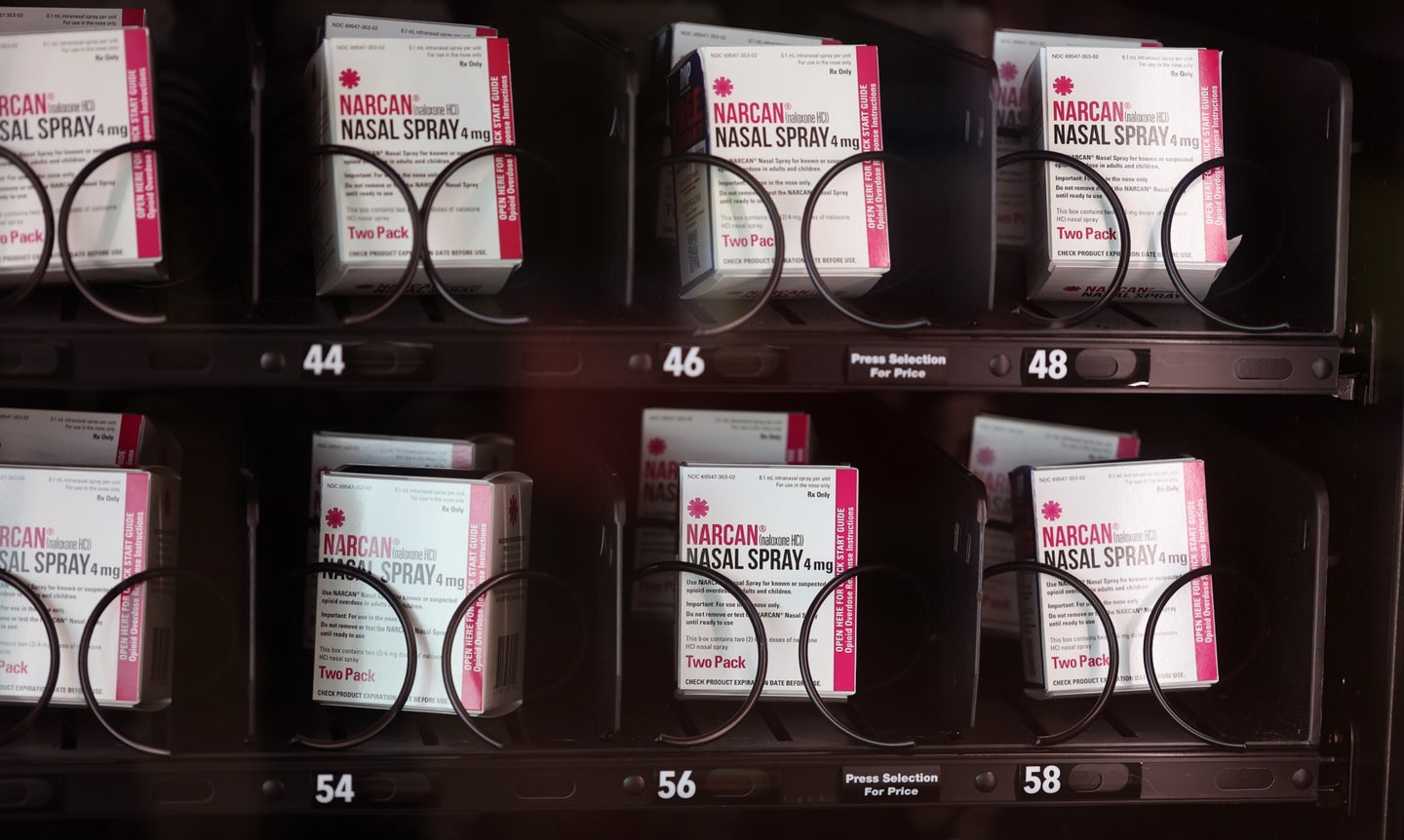
In response to the growing number of opioid overdose deaths—75 percent of drug overdose deaths in the US in 2020 involved an opioid—the Food and Drug Administration (FDA) approved an over-the-counter version of naloxone. The decision makes the drug more accessible: People will be able to buy the nasal spray at places like their local pharmacy or gas station without a prescription. But while medical experts have lauded the FDA’s ruling, not everyone is happy with the news. There have been some concerns from the public about distributing naloxone and whether it encourages more drug use. PopSci spoke with medical experts on common misconceptions surrounding naloxone and its safety.
Myth 1: Naloxone encourages people to do more drugs
A common objection to expanding naloxone access is that it acts as a safety net for people with addiction to continue their drug habits with few repercussions. But Kathryn Cunningham, director of the Center of Addiction Research at the University of Texas Medical Branch, says research has shown no evidence that naloxone leads to more drug use.
A well-known 2013 study in The BMJ journal found the number of opioid-related hospital visits did not increase in communities with programs distributing naloxone and those with less access to the nasal spray. Instead, naloxone helped in reducing the amount of risky drug activity in 19 communities that distributed it to residents.
Myth 2: Naloxone prevents users from getting treated for addiction
Think of naloxone as a fire extinguisher in your house, Marino says. You’ll likely use it if there’s a small blaze. But if you have repeated incidents or if your house becomes engulfed in flames, the fire extinguisher can only help so much. Eventually, you’ll have to call the fire department for help. Simply put, naloxone may actually convince people to find professional help because it gives them more opportunities to seek treatment and rehabilitation later in life. “You can’t seek medical services if you’re dead,” Cunningham explains.
If there’s any deterrent to getting treatment, it’s the stigma surrounding substance use disorders. Research suggests laws hampering access to care and discrimination from medical professionals against patients with a history of drug use may discourage people from opening up about their addiction. Even when they seek out help, patients have reported being treated as if they were untrustworthy, intimidating, and immoral.
Myth 3: Only medical professionals can use naloxone safely
You do not need medical training to give naloxone to someone who’s overdosed. Marino says the over-the-counter nasal spray that the FDA approved was designed to be easy enough to be used by a child as young as 6. The box also has step-by-step instructions printed on the side. “It comes with this little nasal atomizer,” Marino adds. “You just take it out of the package, put it in someone’s nose, and press the pointer. That’s all there is to it.” If a person accidentally applies naloxone to someone who hasn’t overdosed, it will be benign.
[Related: How to break free of the bystander effect and help someone in trouble]
There is no age limit for being treated with naloxone. You can use it on a newborn with opioids in their system or even a toddler who’s exposed to fentanyl patches. The nasal spray expires after three years, and should be stored in temperatures between 77 and 104 degrees Fahrenheit. Naloxone freezes at temperatures below 5 degrees Fahrenheit, making it unusable until it thaws out.
Myth 4: Naloxone makes users violent
It’s been rumored that the sudden onslaught of withdrawal symptoms caused by naloxone might cause a person to become aggressive or lash out when they gain consciousness. That’s not typically the case. Cunningham says common side effects after treatment include headaches, disorientation, vomiting, and nausea—all of which are temporary, because it’s a short-acting drug. “Withdrawal is not life-threatening,” Cunningham notes. “Not breathing because of an opiate is life-threatening.”
Fact: Naloxone could save many lives if more people have it
The FDA’s decision (which doesn’t mention exact rollout dates) makes it so that anyone can be ready to jump in and prevent deaths from opioid overdoses. Marino says it’s best to think of naloxone as another item in your first aid kit in case of emergencies. “We might tell ourselves that no one in our life is using drugs or going to overdose, but you never want to have a situation where you need it and not have it.”