Abstract
Fungal pathogens cause more than a billion human infections every year, resulting in more than 1.6 million deaths annually. Understanding the natural history and evolutionary ecology of fungi is helping us understand how disease-relevant traits have repeatedly evolved. Different types and mechanisms of genetic variation have contributed to the evolution of fungal pathogenicity and specific genetic differences distinguish pathogens from non-pathogens. Insights into the traits, genetic elements, and genetic and ecological mechanisms that contribute to the evolution of fungal pathogenicity are crucial for developing strategies to both predict emergence of fungal pathogens and develop drugs to combat them.
Similar content being viewed by others
Main
With approximately 150,000 species described but perhaps as many as a few million more species awaiting discovery1,2, the kingdom of fungi is the lesser-known of the ‘big’ three eukaryotic kingdoms after animals and plants. Yet fungi are every bit as vital to our lives and the planet as animals and plants. Although fungi are intricately intertwined with human society, they remain largely unappreciated and understudied3,4. Unlike bacterial and viral pathogens, fungi have received less attention in the context of human disease5,6. However, recent data suggest that the global annual burden of fungal disease is enormous; superficial (for example, skin, hair, nail and eye) infections are estimated to affect a billion people, mucosal (for example, oral and vaginal) infections affect approximately 135 million, allergic infections affect about 23.3 million, and chronic severe and acute invasive infections affect several additional millions of people and have extremely high mortality rates7. The mortality rates in certain groups of severely immunocompromised patients with invasive aspergillosis can be as high as 50%8. Fungal diseases are responsible for more than 1.6 million deaths annually, a rate on par with that of tuberculosis and more than three times higher than that of malaria7. These are staggering numbers, especially considering how little is known about the biology of fungal pathogens and the lack of recognition of the effects of fungal infections on human health3,6.
One reason for the lack of attention to fungal pathogens lies in their opportunistic nature. In contrast to bacteria and viruses, fungi only emerged as important human pathogens in the past few decades, primarily owing to changes in the landscape of human disease9 (Fig. 1); these changes include the dramatic increase in the number of immunocompromised patients (owing to mutations that impair host immune function, cancer chemotherapy or the effect of drugs that prevent transplant organ rejection) and the advent of new diseases that seriously compromise immune-system function (for example, AIDS). Unfortunately, but not surprisingly, fungal pathogens cause secondary infections in individuals with severe COVID-19 (Box 1). This opportunistic behaviour also means that many of the traits and genetic elements that make fungal pathogens virulent are not unique or specific disease determinants but have probably evolved for survival in conditions independent of human infection. Therefore, understanding fungal virulence requires understanding of the natural history, ecology and adaptations of fungi that facilitate their success in their natural environments.
This review discusses the where, why and how of the evolution of human fungal pathogenicity. First, the repeated evolution of fungal pathogenicity and where it took place on the fungal tree of life is presented. Next, the opportunistic nature of human fungal pathogens is discussed, including how their ecological traits can help explain why some fungal species infect hundreds of thousands of patients annually, while closely related fungal species are relatively harmless. Finally, this review tackles the question of how fungal pathogenicity evolved by discussing the types of genetic variation that give rise to variation in virulence. Fungal pathogenicity is the outcome of complex interactions between pathogens, human hosts and their environments (Box 2). However, this review does not cover the role of the human immune system10,11,12 or the role of antifungal drug resistance in the evolution of fungal pathogenicity13,14, both of which are important topics and merit discussion in separate reviews.
Fungal pathogenic traits have evolved repeatedly
The kingdom Fungi is extraordinarily diverse and contains more than two hundred orders and a dozen phyla15,16, with new ones being described continuously17. However, the vast majority of infections and deaths caused by fungi result from a few hundred fungal species that belong to a few lineages (Table 1). These human fungal pathogens have evolved repeatedly from non-pathogens across major lineages of the fungal tree of life (Fig. 2). Plotting the genera harbouring the major human pathogens on the fungal tree of life reveals that human pathogenicity has evolved in more than a dozen different lineages. Interestingly, pathogenicity has also evolved repeatedly within some of these lineages, suggesting that they may harbour traits that pre-adapt them to human pathogenicity. For instance, pathogenicity has evolved multiple times independently in Aspergillus fungi18. As such, the closest relatives of the two major pathogens causing aspergillosis—that is, Aspergillus fumigatus (Fig. 3) and Aspergillus flavus—are non-pathogenic19,20,21. Human pathogenicity has also evolved independently within Onygenales, the order that contains dermatophytes and dimorphic fungi22, as well as within Mucorales, which harbours the causative agents (Mucor, Rhizopus and their relatives) of the devastating disease mucormycosis23. Similarly, pathogenicity has evolved independently at least five times within budding yeasts24,25, including in the causative agents of candidiasis Candida (Nakaseomyces) glabrata and Candida albicans and in the emerging pathogen Candida auris (Fig. 2).
Genera and lineages harbouring major and emerging fungal pathogens (see Table 1) are shown in red and non-pathogenic taxa are shown in black. Fungal tree of life based on a phylogenomic analysis of 1,644 species and 290 genes from ref. 16. Only species whose genomes have been sequenced are included. The tree with species names included is shown in Supplementary Fig. 1. Figure adapted with permission from ref. 16, Elsevier.
Biosafety level-2 species are considered pathogenic and are shown in red. Biosafety level-1 organisms are shown in black. The estimated number of cases of invasive infection per year are shown in parentheses. Phylogeny modified from refs. 18,139,140,141; infection case estimates from refs. 7,142. Figure adapted with permission from ref. 18, under a Creative Commons license CC BY 4.0.
In some instances, several species within a lineage are human pathogens. These closely related pathogenic fungi often exhibit substantial differences in their pathogenicity. Although C. albicans and its closest known relative Candida dubliniensis are both human pathogens, C. albicans is much more virulent than C. dubliniensis26. Similarly, the closely related pathogenic species in the genus Cryptococcus, which cause the potentially lethal fungal disease cryptococcosis, display substantial variation in their virulence and pathogenicity (Box 2)—Cryptococcus neoformans primarily infects immunocompromised individuals, whereas Cryptococcus gattii infections primarily affect immunocompetent individuals27,28. The dozen pathogenic species in the Aspergillus section Fumigati also display considerable variation in their virulence and antifungal drug-resistance profiles29.
Differences in the pathogenicity of closely related species can be observed in large lineages of major pathogenic species such as in Malassezia—a genus of basidiomycete yeasts that contains several species adapted to living on the human skin30—as well as in the dermatophytes and dimorphic fungi in the order Onygenales. Onygenales harbours several different genera of so-called thermally dimorphic fungi, such as Blastomyces, Coccidioides, Histoplasma and Paracoccidioides, which grow in mycelial form in typical environmental temperatures (for example, 25 °C) but switch to yeast growth at human body temperature. These dimorphic fungi differ widely in their pathogenicity and disease profiles31. Another clade within Onygenales harbours multiple genera of dermatophyte fungi (such as Trichophyton, Epidermophyton and Microsporum) that can cause skin infections and exhibit a wide variation in pathogenicity32.
Variation or heterogeneity in pathogenicity-associated genes and traits is not restricted between species and lineages but is also observed among strains within populations of fungal pathogens. This strain heterogeneity is both evolutionarily interesting (for example, for revealing the genetic or epigenetic mechanisms that contribute to the evolution of pathogenicity) and clinically relevant (for example, different strains often exhibit different virulence and antifungal drug-resistance profiles). Strains of C. albicans33,34, A. fumigatus35,36,37 and other Aspergillus pathogens38 exhibit extensive genomic and phenotypic heterogeneity in their virulence and drug-resistance profiles. Similarly, genetic diversity within the major pathogen C. neoformans is associated with patient clinical outcome39. Not much is known about the extent of this strain heterogeneity and how it may be influenced by differences in the sampling of strains between species or how species boundaries are defined. However, studies in Aspergillus have shown that the amount of variation in virulence observed within a major pathogen is lower than that observed between the pathogen and its non-pathogenic closest relatives20,36,37.
As mentioned earlier, a relatively small number of fungal species are considered major pathogens (Fig. 2). However, it is worth noting that the spectrum of fungi capable of causing disease is probably much larger and nearly every fungus can be an opportunistic or accidental pathogen in a human host whose immune system is severely weakened (see also Box 2). Support for this hypothesis comes from clinical case reports of invasive infections by diverse well-known species of fungi that are thought to be harmless to humans. These include the baker’s yeast Saccharomyces cerevisiae40, the splitgill mushroom Schizophyllum commune41, the grey shag Coprinopsis cinerea42 and the basidiomycete pigmented yeasts in the genus Rhodotorula43.
Human pathogenic fungi have originated independently multiple times across the fungal kingdom as well as within certain lineages, which highlights the remarkable versatility of these organisms and their ability to colonize new ecological niches, like those provided by human hosts. It should be noted that most of the human pathogenic fungi, such as pathogenic species in the genera Aspergillus, Candida, Cryptococcus, Histoplasma and Coccidioides, also infect many other animals, including other vertebrates and mammals44. These animal infections, much like human infections, are caused via direct acquisition of fungal spores from the environment, but zoonotic outbreaks with direct transmission from animals to humans (for example, cat to human transmission of Sporothrix brasiliensis45) are also known44. Thus, much like human pathogenicity (Fig. 2), animal pathogenicity has also evolved multiple times independently across the fungal tree of life. Of course, the ability to cause disease in humans and the ability to cause disease in other warm-blooded animals are tightly linked as both rely on certain infection-relevant traits, such as thermotolerance (see the next section). Are these infection-relevant traits shared by human pathogens across the fungal tree of life? Answering this major question requires understanding the life cycle of a typical fungal infection and its opportunistic nature, which is discussed in the next section.
Ecological traits that aid opportunistic pathogenicity
Human pathogenic fungi differ greatly with respect to their degree of adaptation to their pathogenic lifestyles. At the one end of the spectrum one finds obligate pathogens such as Microsporidia, a phylum of unicellular fungi that are intracellular parasites of a wide range of animal hosts46. Passage through a host is a required part of the microsporidian life cycle and these pathogens have probably co-evolved with their hosts and possess adaptations for within-host survival. In the middle of the spectrum one finds organisms that have a commensal relationship with their hosts. For instance, the extracellular Pneumocystis yeasts cannot survive outside of a mammalian host (that is, they are host-obligate), turning pathogenic in hosts with weakened immune systems47. Budding yeasts that cause candidiasis are also commensal48, although they are not host-obligate and recent studies have shown that these species are also present in the natural environment25,49. It is probable that these commensals-turned-pathogens have also co-evolved, at least to some extent, with humans (in the case of budding yeasts) and mammals (in the case of Pneumocystis).
However, the majority of the approximately 200 fungal pathogens that infect humans9 lie at the other end of the spectrum; they are typically not dependent on their hosts for survival and growth, and their pathogenicity is accidental or opportunistic50,51. In nature, fungi are the primary decomposers of organic matter, growing on a variety of substrates and interacting with a wide range of organisms. Because most fungal pathogens are opportunistic, we can gain insight into their ability to infect humans by considering their natural environments. Soil, for example, is a common ecological niche where many opportunistic pathogenic fungi can be found. A single gram of soil harbours billions of microbial organisms from thousands of species belonging to dozens of taxonomic groups52. Survival in such a highly competitive environment requires many adaptations related to defence, feeding and growth, and it has been argued that pathogenicity-associated traits are precisely those that also facilitate fungal survival in nature53,54. A recent evolutionary ecological examination of more than 1,200 fungal species revealed a significant association between the ability to survive in multiple different types of extreme conditions (thermotolerance, osmotolerance and so on) and opportunistic pathogenicity55. For example, ascomycete fungi tend to be more widely distributed and thermotolerant than basidiomycete fungi56,57, which may be partly explain why there are more lineages of opportunistic human pathogens in ascomycetes than in basidiomycetes (Fig. 2 and Table 1).
These observations suggest that understanding why fungi are such successful opportunistic pathogens will require detailed understanding of the natural fungal lifestyle and the ways in which the human host environment parallels their natural environment. One way to begin addressing this question is by examining the traits that distinguish pathogens from their non-pathogenic relatives. Differences in fungal pathogenicity may stem from variation in a wide variety of ecological traits, such as distribution and abundance56,58, ability to grow at human body temperature57, ability to adapt to varying levels of oxygen59, preference for sexual versus asexual reproduction60 and their response to natural predators61.
If certain ecological traits are infection-relevant, it follows that we should expect human pathogens and their most closely related non-pathogenic relatives to exhibit significant differences in these traits. Although most research so far has focused on just the pathogens, comparisons between pathogenic species and their non-pathogenic relatives provide support for this prediction. For example, the major pathogen A. fumigatus grows better at human body temperature and is much more tolerant to oxidative stress or stress associated with nutrient and oxygen availability than its very close non-pathogenic relative Aspergillus fischeri20. Differences in the ability to grow at human body temperature are also observed between organisms in the pathogenic Cryptococcus species complex, which includes the major pathogens C. neoformans and C. gattii, as well as their closely related non-pathogenic relatives, such as Cryptococcus amylolentus62,63.
Closely related pathogens also exhibit differences in ecological traits associated with human pathogenicity. The pathogens C. neoformans and C. gattii differ substantially in their ecology (C. neoformans is more often associated with bird infections, whereas C. gattii with mammal infections), thermotolerance and melanin production27. For human skin commensals, such as Malassezia yeasts and dermatophytes, different species are typically associated with different body sites30,64. Even in cases where little is known about the natural history of a lineage that harbours pathogenic species, the available evidence is suggestive of key differences in ecology. For example, the three most common causative agents of sporotrichosis—S. brasiliensis, S. schenckii and S. globosa—show substantial differences in their geographical distribution and transmission routes65. S. globosa, which is most prevalent in Asia, is commonly isolated from plant material and wounds caused by such material are the main route of S. globosa human infection on this continent; infections by S. schenckii, which is most common in South Africa and Australia, also typically stem from an environmental transmission route45. In contrast, the main route for human infections by S. brasiliensis, which is most prevalent in Brazil, is via infected domestic animals such as cats and dogs45.
Examination of some of these ecological traits has been key to our understanding of fungal pathogenicity and how it may have evolved. Many opportunistic fungal pathogens are saprophytic organisms that live in the soil where they are predated on by diverse organisms, such as amoebae, whose functions in the natural environment can be perceived to parallel those of phagocytes in the human host environment66. This hypothesis, which was first raised and tested in 2001 with C. neoformans, yielded two striking results: first, the fungal interactions with amoebae were similar to interactions of the fungus with macrophages and second, several traits, such as melanization, that contribute to fungal resistance against mammalian immune cells also provide protection from amoeba predation66. These discoveries have spearheaded a body of work examining how the coevolution of fungi with their natural predators may have accidentally favoured or selected for the evolution of human pathogenicity and ability to withstand host defence strategies61,67 not just in Cryptococcus68,69 but also in other soil fungi, such as Aspergillus61 and Paracoccidioides70. A recent examination of the interactions between Paracoccidioides opportunistic fungal pathogens and their natural amoeba predators showed that repeated exposure of Paracoccidioides to predatory amoebae increased the ability of these fungi to survive mammalian macrophages and to infect mice70. Interestingly, studies on Cryptococcus have shown that prolonged growth in the presence of predatory amoebae selected for mutations that promote pseudohyphal (rather than yeast) growth, which increase resistance to macrophages but reduce virulence68,69. Data are lacking on whether this variation is observed in the natural environment but raise the hypothesis that interactions of fungi with other organisms may generate substantial phenotypic diversity that is relevant for the capacity of individual strains to infect humans.
One prediction that follows from the repeated evolution of human pathogenic fungi is that several of their infection-relevant ecological traits may also have evolved repeatedly (convergent evolution). For example, thermotolerance is widely regarded as a key trait for fungal pathogens of humans and other warm-blooded animals, and harbours this signature of convergent evolution57. Another trait that has repeatedly evolved in human pathogenic fungi is osmotolerance55. One particularly noteworthy example of convergent evolution is the developmental ability of certain human pathogenic fungi to switch between filamentous (or mycelial) and yeast growth, which has evolved multiple times independently across multiple fungal phyla71 and is observed in diverse pathogens, including C. albicans and C. neoformans. Some of the most notable examples of organisms that exhibit this morphogenetic switch are the thermally dimorphic fungi that have independently evolved in the orders Onygenales (for example, Histoplasma¸ Blastomyces, Coccidioides and Paracoccidioides) and Ophiostomatales (which includes Sporothrix); the trait also evolved independently in Talaromyces marneffei (order Eurotiales)72. In these thermally dimorphic fungi, the switch from filamentous to yeast growth during infection confers protection against host defence responses72. Interestingly, whereas thermal dimorphism is widespread in the orders Onygenales and Ophiostomatales, only a single species from the order Eurotiales (T. marneffei) is known to be dimorphic71.
Once associated with human hosts, fungal survival and reproductive strategies may quickly diverge from strategies favoured when they are in their natural environments. Comparisons of clinical and environmental strains of S. cerevisiae have revealed that clinical strains show higher levels of heterozygosity, a reduced ability for sexual reproduction and an increased propensity for pseudohyphal development than environmental strains60,73.
Finally, it is worth noting the potential limitation of this evolutionary approach, namely the assumption that diverse fungal pathogens share infection-relevant ecological traits. Although the examples discussed above suggest that this is indeed the case for traits such as thermotolerance and osmotolerance, the question remains whether there are other convergent traits shared by opportunistic human fungal pathogens. A non-mutually exclusive alterative is that understanding of fungal pathogenicity will require a detailed dissection of the interactions of each pathogen with the human host because each pathogen has its own unique suite of infection-relevant ecological traits. One notable example of this alternative hypothesis is secondary metabolites, which are small, bioactive molecules biosynthesized by certain fungi that play key roles to their ecology. Secondary metabolites produced by fungal pathogens such as A. fumigatus have been shown to influence host biology and pathogenicity74. However, the ability of several other pathogens to biosynthesize secondary metabolites is either limited (for example, C. albicans and C. neoformans) or is reduced relative to their non-pathogenic relatives (for example, dimorphic fungi75).
Bridging evolutionary analyses with targeted genetic studies can elucidate the genetic basis of several infection-relevant ecological traits in fungal pathogens and help refine our concept of how fungal pathogenicity evolves. The next section describes how genetic variation associated with these traits has contributed to the evolutionary origin and maintenance of fungal pathogenicity.
Fungal genomics and human pathogenicity
Fungal pathogenicity is the outcome of complex interactions between the pathogens, human hosts (immune-system status of the host) and their environment (for example, spore availability; Box 2). Although host genetics, host immune-system status and environment certainly contribute to the manifestation of fungal disease, differences in genetic elements associated with infection-relevant ecological traits are also major contributors. Genetic variants that have contributed to the evolution of fungal pathogenicity can be broken down into two broad categories or types: larger-scale genomic changes that affect the entire genome or large parts of it—such as hybridization76, introgression77, transposon mobilization78, loss of heterozygosity79 and variation in ploidy79—and smaller-scale changes that typically affect a single genomic region—such as copy number variation80, gene duplication81, gene loss75, horizontal gene transfer82, indels and single nucleotide polymorphisms33 (Fig. 4). It is also important to emphasize the remarkable plasticity of fungal genomes with respect to the range of mechanisms and processes that can give rise to this genetic variation, including the diversity of their reproductive strategies83.
a–e, Some of the types of genetic variation that typically affect large genomic regions or entire genomes are illustrated; these include variation in ploidy (a), loss of heterozygosity (b), transposon mobilization (c), introgression (d) and hybridization (e). In a,b, the yellow and blue colours represent the two sets of homologous chromosomes. In d,e, the letters represent different taxa. In d, the green arrow illustrates the introgression of a genomic region from taxon B into the genome of taxon C. In e, the red branch leading to taxon D is meant to illustrate the origin of a new hybrid. f–i, Other types of variation typically affect a single locus; these include copy number variation (f), horizontal gene transfer (g), single nucleotide polymorphisms (h), cis-regulatory-element variation (i) and gene duplication and loss (j). f, Copy number variation could involve linear or circular DNA. In j, the red and blue lines denote the differential fates of a pair of duplicate genes. In i, the coloured boxes correspond to different cis-regulatory elements and the arrows to the gene transcription start sites. Most identified examples of genetic variation concerning the evolution of human fungal pathogens focus on or concern variation in the protein-coding regions of the genome (a–h,j). However, variation of cis-regulatory elements, which can alter gene activity, can also have a major impact in the evolution of fungal pathogens (i). We currently lack understanding of the relative frequency with which these mechanisms operate in different fungal pathogens. It is also probable that these mechanisms differ in their prevalence in fungal genomes. Figure adapted with permission from: a,b, ref. 162, American Society for Microbiology; c, ref. 163, Springer Nature Ltd; d,e, ref. 164, Springer Nature Ltd; f, reprinted courtesy of the National Human Genome Research Institute, https://www.genome.gov; g, ref. 165, Springer Nature Ltd; h, ref. 166, Springer Nature Ltd; i, ref. 167, under a Creative Commons license CC BY 4.0; j, ref. 168, under a Creative Commons license CC BY 4.0.
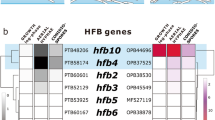
Comparisons of the genomes of pathogenic fungi and their non-pathogenic relatives have identified numerous large- and small-scale genomic differences associated with the origins of pathogenicity, implicating many genes with diverse functions84. One notable difference between thermally dimorphic fungal pathogens and their non-pathogenic relatives is that pathogens have lost secondary metabolic genes and genes associated with the degradation of plant material75. Similarly, a recent comparative genomic examination of the host-obligate Pneumocystis species revealed extensive between-species variation in the msg superfamily, whose members are involved in pathogen–host interactions81. An examination of horizontal gene transfer in Malassezia identified more than two dozen genes that were probably acquired from bacteria, including a flavohaemoglobin-encoding gene, which was shown to be involved in nitric oxide resistance and interaction with the human host82. Comparisons between pathogenic and closely related non-pathogenic Aspergillus species have revealed extensive differences in the presence of biosynthetic gene clusters involved in secondary metabolite biosynthesis85; several of these bioactive small molecules are known to be important to Aspergillus ecology and to modulate human host biology74.
Although many of the known variants are from the protein-coding parts of the genome, differences in the regulation of genes that are conserved in both pathogens and non-pathogens can also contribute to differences in pathogenicity. As mentioned earlier, C. albicans and C. dubliniensis differ in their virulence but are very closely related and do not contain many differences in gene content86. However, a systematic examination of differences in gene expression of orthologous genes between the two species revealed that all 15 genes involved in glycolysis were more highly expressed in C. albicans than in C. dubliniensis26. Strikingly, genetic engineering of a C. dubliniensis strain that expressed all 15 glycolysis genes at higher-than-native levels led to an increase in virulence26. Thus, much like the case for other traits87,88, changes in pathogenicity and infection-relevant traits may stem from genetic changes in both the protein-coding and regulatory parts of the genome.
Genetic variants associated with pathogenicity are also found in examinations of within-species variation, an observation in line with the heterogeneity in infection-relevant traits seen between strains of individual fungal pathogenic species. Strains of the major pathogen A. fumigatus show variation in the structure of their biofilms, which influences the ability of strains to grow in low-oxygen environments, such as that encountered inside human lungs. Interestingly, this variation stems from variation in the presence of the hrmA gene across A. fumigatus strains35. Similarly, examination of genomic variation in strains of the major pathogen C. albicans identified numerous genetic changes, including single nucleotide polymorphisms, that contributed to strain variation in virulence and other infection-relevant traits33. Comparison of clinical and environmental S. cerevisiae strains revealed higher levels of heterozygosity in the clinical strains and identified significant associations between specific genetic variants and pathogenicity-associated phenotypes, such as increased copper resistance60,73.
Looking into the past and reconstructing how pathogenicity evolved using comparative genomics is one approach towards understanding the observed differences between pathogens and non-pathogens. An independent approach is to ask how pathogenicity could evolve, which can be achieved through experimental evolution approaches89. Such experiments typically select (over many generations) those individuals in a fungal population that show increased survival or growth in a particular environment (such as the oral cavity90) or that exhibit a particular infection-relevant trait (such as thermotolerance91 and reduction92 or increase of virulence93). Repeated passage of environmentally derived isolates of C. neoformans through mice results in significant increases in virulence93. This is, at least partly, due to the higher expression of the FRE3 gene, which encodes for an iron reductase. In the commensal C. albicans, experimental evolution for loss of virulence via repeated passaging through a mammalian host identified key genes and traits associated with the transition from commensalism to mutualism92. In addition, repeated passage of the same species through the oral cavity90 and gastrointestinal tract94 of mice led to the identification of a chromosome 6 trisomy that was shown to result in a commensal-like phenotype (in the oral cavity experiment95) and a chromosome 7 trisomy that increased fitness in the gastrointestinal tract94.
Finally, it is worth noting that some of the examples mentioned concern genetic mechanisms that contributed to the origin of human (and/or animal) pathogenicity in the first place (for example, gene content variation stemming from differential gene duplication and loss between pathogens and their non-pathogenic close relatives). Other examples concern genetic mechanisms that shaped adaptation during evolution inside the human host or in response to interventions, such as treatment with antifungal drugs (for example, variation in ploidy, heterozygosity and gene copy number). We currently lack an understanding of the relative frequency with which these mechanisms operate in different fungal pathogens and their relative importance for the origin of pathogens versus the maintenance of the human pathogenic lifestyle.
Outlook
In the last two decades, adoption of an ecological and evolutionary perspective, coupled with the huge advances in genomics, has revolutionized medical mycology83,84, greatly illuminating the broad contours of the where, why and how of the evolution of fungal pathogenicity. But several major gaps remain, including our understanding of the genetic and ecological factors that contribute to the emergence of new human fungal pathogens. In a planet with a rapidly changing climate that has witnessed the emergence of several new pathogens (Box 3), forecasting the emergence of new pathogens is becoming more urgent than ever9,51. Understanding how pathogens evolve as well as figuring out the genetic determinants that contribute to the origin and maintenance of fungal pathogenicity could aid in the identification of potential vulnerabilities that could be targeted for new therapeutics13,14. Three grand challenges that, if tackled, promise to greatly advance our understanding of the origins of fungal pathogens of humans, potentially facilitating the development of models that predict the emergence of new ones and of therapeutics that better combat fungal infections are discussed below.
The challenge of understanding fungal biodiversity and ecology
This is arguably the biggest knowledge gap, especially considering the opportunistic nature of most major fungal pathogens and the frequent emergence of new ones. We still lack a fundamental understanding of the diversity of fungal species1,2,96. Even for the small fraction of species that are known to science, including most fungal pathogens, we do not typically know their natural distribution and ecological niches or how pathogenic and non-pathogenic fungi interact with other organisms in nature. Although some of that knowledge is available for certain pathogens (for example, the natural reservoirs of T. marneffei in wild rodents are well-defined, linking the ecology of the organism with disease epidemiology97), it is lacking for many others, hindering efforts to understand their biology and epidemiology. For instance, we do not know the environmental reservoirs, if any, of Pneumocystis species98, the zoonotic reservoirs for many microsporidian human pathogens46 or the ecology of the emerging Sporothrix human pathogens65.
The challenge of systematically characterizing pathogens and non-pathogens
In most lineages harbouring pathogens and their non-pathogenic relatives, we lack data on the phenotypic profiles of the non-pathogens and their growth characteristics in infection-relevant conditions; for many non-pathogenic relatives of major pathogens (such as C. glabrata99 and A. fumigatus18), there is a paucity of data on their ability to grow at 37 °C and their tolerance to various infection-relevant stresses. This lack of systematic data collection with respect to fungal biodiversity and ecology as well as characterization of pathogens and non-pathogens makes it difficult to begin to understand and make predictions of where new human pathogens are more likely to emerge from. From lineages that are thermotolerant or extremotolerant? From lineages that harbour fungal pathogens of other mammals? From lineages that live in extremely competitive environments or are widely distributed geographically? Temperature growth assays have shown that species in the pathogenic C. neoformans or C. gattii clade have the capacity to grow at human body temperature, whereas their closely related non-pathogenic relatives do not, suggesting that the ability to grow at human body temperature evolved in the ancestor of the pathogen clade. Thus, evolution of thermotolerance is tightly coupled to the evolution of pathogenicity in Cryptococcus, but whether this pattern is observed in other clades containing fungal pathogens remains unknown. Although several hypotheses have been proposed and associations have been drawn, systematic testing of these hypotheses is lacking, largely because of the historical unavailability of large synthetic datasets that contain the high-quality data necessary to address these questions. Large-scale datasets of genomic100, evolutionary16,101,102, taxonomic103 and ecological104 diversity of fungi are going to be invaluable in this synthesis.
The challenge of understanding the relationship between genotype and phenotype for pathogenicity- and virulence-related genes and traits
The amount of genomic and phenotypic variation or heterogeneity in pathogenicity across human fungal pathogens remains largely unknown. Research in S. cerevisiae, where clinical strains show a reduced ability for sexual reproduction and an increased propensity for pseudohyphal development, raises the hypothesis that fungal survival and reproductive strategies favoured inside human hosts will be distinct from those in their natural environments60,73, but we still lack understanding of the degree and speed with which fungi can alter these key traits to adapt to the human host environment. We also lack understanding of how much of the observed phenotypic variation has a genetic basis, and the heritability of most infection-relevant traits in most pathogens remains unknown. This makes it challenging to infer what cellular pathways should be targeted for the development of fungal vaccines and antifungal drugs. For example, a recent study showed that genetically identical asexual spores of different fungal species, including those of the pathogens A. fumigatus and T. marneffei, exhibit substantial phenotypic diversity105. However, diverse approaches are now available to study the proportion of phenotypic variation that stems from genetic variation, including genome-wide association studies106,107, reverse ecology84 as well as a range of phylogenetic methods108. These analyses can link the genotypic and phenotypic variation observed not only within but also between fungal species.
Conclusion
Now that fungal genomes can be sequenced in the hundreds and thousands, and tools that enable the genetic and molecular dissection of infection-relevant traits have been developed, the limiting factor in tackling pathogenic fungi is a better understanding of fungal ecology and natural history. Which lineages and ecological lifestyles will human fungal pathogens emerge from? What are the key genetic and ecological differences that distinguish pathogenic fungi from their non-pathogenic relatives? Answering these vital questions will require the synthesis of genomic, evolutionary and ecological features of fungal lineages.
References
Blackwell, M. The fungi: 1, 2, 3… 5.1 million species? Am. J. Bot. 98, 426–438 (2011).
Hawksworth, D. L. & Lucking, R. Fungal diversity revisited: 2.2 to 3.8 million species. Microbiol. Spectr. https://doi.org/10.1128/microbiolspec.FUNK-0052-2016 (2017).
Stop neglecting fungi. Nat. Microbiol. https://doi.org/10.1038/nmicrobiol.2017.120 (2017).
Fungus focus. Nat. Ecol. Evol. https://doi.org/10.1038/s41559-018-0721-1 (2018).
Denning, D. W. Calling upon all public health mycologists: to accompany the country burden papers from 14 countries. Eur. J. Clin. Microbiol. Infect. Dis. 36, 923–924 (2017).
Konopka, J., Casadevall, A., Taylor, J., Heitman, J. & Cowen, L. One Health: Fungal Pathogens of Humans, Animals, and Plants (American Academy of Microbiology, 2019).
Bongomin, F., Gago, S., Oladele, R. O. & Denning, D. W. Global and multi-national prevalence of fungal diseases-estimate precision. J. Fungi 3, 57 (2017).
Latge, J. P. & Chamilos, G. Aspergillus fumigatus and aspergillosis in 2019. Clin. Microbiol. Rev. https://doi.org/10.1128/CMR.00140-18 (2019).
Fisher, M. C. et al. Threats posed by the fungal kingdom to humans, wildlife, and agriculture. mBio 11, e00449-20 (2020).
Chang, C. C. & Levitz, S. M. Fungal immunology in clinical practice: magical realism or practical reality? Med. Mycol. 57, S294–S306 (2019).
Gow, N. A. & Netea, M. G. Medical mycology and fungal immunology: new research perspectives addressing a major world health challenge. Philos. Trans. R. Soc. B 371, 20150462 (2016).
Romani, L. Immunity to fungal infections. Nat. Rev. Immunol. 11, 275–288 (2011).
Fisher, M. C., Hawkins, N. J., Sanglard, D. & Gurr, S. J. Worldwide emergence of resistance to antifungal drugs challenges human health and food security. Science 360, 739–742 (2018).
Robbins, N., Caplan, T. & Cowen, L. E. Molecular evolution of antifungal drug resistance. Annu. Rev. Microbiol. 71, 753–775 (2017).
James, T. Y., Stajich, J. E., Hittinger, C. T. & Rokas, A. Toward a fully resolved fungal tree of life. Annu. Rev. Microbiol. 74, 291–313 (2020).
Li, Y. et al. A genome-scale phylogeny of the kingdom Fungi. Curr. Biol. 31, 1653–1665 (2021).
Wijayawardene, N. N. et al. Outline of fungi and fungus-like taxa. Mycosphere 11, 1060–1456 (2020).
Rokas, A., Mead, M. E., Steenwyk, J. L., Oberlies, N. H. & Goldman, G. H. Evolving moldy murderers: Aspergillus section Fumigati as a model for studying the repeated evolution of fungal pathogenicity. PLoS Pathog. 16, e1008315 (2020).
Mead, M. E. et al. An evolutionary genomic approach reveals both conserved and species-specific genetic elements related to human disease in closely related Aspergillus fungi. Genetics 218, iyab066 (2021).
Mead, M. E. et al. Characterizing the pathogenic, genomic, and chemical traits of Aspergillus fischeri, a close relative of the major human fungal pathogen Aspergillus fumigatus. mSphere 4, e00018-19 (2019).
Steenwyk, J. L., Shen, X. X., Lind, A. L., Goldman, G. H. & Rokas, A. A robust phylogenomic time tree for biotechnologically and medically important fungi in the genera Aspergillus and Penicillium. mBio 10, e00925-19 (2019).
Garcia Garces, H., Hamae Yamauchi, D., Theodoro, R. C. & Bagagli, E. PRP8 intein in onygenales: distribution and phylogenetic aspects. Mycopathologia 185, 37–49 (2020).
Hassan, M. I. A. & Voigt, K. Pathogenicity patterns of mucormycosis: epidemiology, interaction with immune cells and virulence factors. Med. Mycol. 57, S245–S256 (2019).
Gabaldon, T., Naranjo-Ortiz, M. A. & Marcet-Houben, M. Evolutionary genomics of yeast pathogens in the Saccharomycotina. FEMS Yeast Res. 16, fow064 (2016).
Opulente, D. A. et al. Pathogenic budding yeasts isolated outside of clinical settings. FEMS Yeast Res. 19, foz032 (2019).
Singh-Babak, S. D., Babak, T., Fraser, H. B. & Johnson, A. D. Lineage-specific selection and the evolution of virulence in the Candida clade. Proc. Natl Acad. Sci. USA 118, e2016818118 (2021).
Hagen, F. et al. Importance of resolving fungal nomenclature: the case of multiple pathogenic species in the cryptococcus genus. mSphere https://doi.org/10.1128/mSphere.00238-17 (2017).
Kwon-Chung, K. J. et al. The case for adopting the ‘Species Complex’ nomenclature for the etiologic agents of cryptococcosis. mSphere https://doi.org/10.1128/mSphere.00357-16 (2017).
Sugui, J. A. et al. Genetic relatedness versus biological compatibility between Aspergillus fumigatus and related species. J. Clin. Microbiol. 52, 3707–3721 (2014).
Grice, E. A. & Dawson, T. L. Jr Host–microbe interactions: Malassezia and human skin. Curr. Opin. Microbiol. 40, 81–87 (2017).
Van Dyke, M. C. C., Teixeira, M. M. & Barker, B. M. Fantastic yeasts and where to find them: the hidden diversity of dimorphic fungal pathogens. Curr. Opin. Microbiol. 52, 55–63 (2019).
de Hoog, G. S. et al. Toward a novel multilocus phylogenetic taxonomy for the dermatophytes. Mycopathologia 182, 5–31 (2017).
Hirakawa, M. P. et al. Genetic and phenotypic intra-species variation in Candida albicans. Genome Res. 25, 413–425 (2015).
Wang, J. M. et al. Intraspecies transcriptional profiling reveals key regulators of Candida albicans pathogenic traits. mBio https://doi.org/10.1128/mBio.00586-21 (2021).
Kowalski, C. H. et al. Fungal biofilm morphology impacts hypoxia fitness and disease progression. Nat. Microbiol. 4, 2430–2441 (2019).
Kowalski, C. H. et al. Heterogeneity among isolates reveals that fitness in low oxygen correlates with Aspergillus fumigatus virulence. mBio https://doi.org/10.1128/mBio.01515-16 (2016).
Ries, L. N. A. et al. Nutritional heterogeneity among Aspergillus fumigatus strains has consequences for virulence in a strain- and host-dependent manner. Front. Microbiol. 10, 854 (2019).
Dos Santos, R. A. C. et al. Genomic and phenotypic heterogeneity of clinical isolates of the human pathogens Aspergillus fumigatus, Aspergillus lentulus, and Aspergillus fumigatiaffinis. Front. Genet. 11, 459 (2020).
Beale, M. A. et al. Genotypic diversity is associated with clinical outcome and phenotype in cryptococcal meningitis across Southern Africa. PLoS Negl. Trop. Dis. https://doi.org/10.1371/journal.pntd.0003847 (2015).
Ventoulis, I. et al. Bloodstream infection by Saccharomyces cerevisiae in two COVID-19 patients after receiving supplementation of Saccharomyces in the ICU. J. Fungi https://doi.org/10.3390/jof6030098 (2020).
Hoenigl, M. et al. Sinusitis and frontal brain abscess in a diabetic patient caused by the basidiomycete Schizophyllum commune: case report and review of the literature. Mycoses 56, 389–393 (2013).
Nanno, S. et al. Disseminated Hormographiella aspergillata infection with involvement of the lung, brain, and small intestine following allogeneic hematopoietic stem cell transplantation: case report and literature review. Transpl. Infect. Dis. 18, 611–616 (2016).
Ioannou, P., Vamvoukaki, R. & Samonis, G. Rhodotorula species infections in humans: a systematic review. Mycoses 62, 90–100 (2019).
Seyedmousavi, S. et al. Fungal infections in animals: a patchwork of different situations. Med. Mycol. 56, 165–187 (2018).
Rodrigues, A. M., de Hoog, G. S. & de Camargo, Z. P. Sporothrix species causing outbreaks in animals and humans driven by animal–animal transmission. PLoS Pathog. 12, e1005638 (2016).
Han, B., Pan, G. & Weiss, L. M. Microsporidiosis in humans. Clin. Microbiol. Rev. https://doi.org/10.1128/CMR.00010-20 (2021).
Cushion, M. T. Are members of the fungal genus Pneumocystis (a) commensals; (b) opportunists; (c) pathogens; or (d) all of the above? PLoS Pathog. 6, e1001009 (2010).
Romo, J. A. & Kumamoto, C. A. On commensalism of Candida. J. Fungi https://doi.org/10.3390/jof6010016 (2020).
Bensasson, D. et al. Diverse lineages of Candida albicans live on old oaks. Genetics 211, 277–288 (2019).
Taylor, L. H., Latham, S. M. & Woolhouse, M. E. Risk factors for human disease emergence. Philos. Trans. R. Soc. B 356, 983–989 (2001).
Fisher, M. C. et al. Emerging fungal threats to animal, plant and ecosystem health. Nature 484, 186–194 (2012).
Fierer, N. Embracing the unknown: disentangling the complexities of the soil microbiome. Nat. Rev. Microbiol. 15, 579–590 (2017).
Tekaia, F. & Latge, J. P. Aspergillus fumigatus: saprophyte or pathogen? Curr. Opin. Microbiol. 8, 385–392 (2005).
Casadevall, A. Cards of virulence and the global virulome for humans. Microbe 1, 359–364 (2006).
Gostincar, C. et al. Fungi between extremotolerance and opportunistic pathogenicity on humans. Fungal Diversity 93, 195–213 (2018).
Egidi, E. et al. A few Ascomycota taxa dominate soil fungal communities worldwide. Nat. Commun. 10, 2369 (2019).
Robert, V., Cardinali, G. & Casadevall, A. Distribution and impact of yeast thermal tolerance permissive for mammalian infection. BMC Biol. 13, 18 (2015).
Yamamoto, N. et al. Particle-size distributions and seasonal diversity of allergenic and pathogenic fungi in outdoor air. ISME J. 6, 1801–1811 (2012).
Chung, H. & Lee, Y. H. Hypoxia: a double-edged sword during fungal pathogenesis? Front. Microbiol. 11, 1920 (2020).
Magwene, P. M. et al. Outcrossing, mitotic recombination, and life-history trade-offs shape genome evolution in Saccharomyces cerevisiae. Proc. Natl Acad. Sci. USA 108, 1987–1992 (2011).
Novohradska, S., Ferling, I. & Hillmann, F. Exploring virulence determinants of filamentous fungal pathogens through interactions with soil amoebae. Front. Cell. Infect. Microbiol. 7, 497 (2017).
Bloom, A. L. M. et al. Thermotolerance in the pathogen Cryptococcus neoformans is linked to antigen masking via mRNA decay-dependent reprogramming. Nat. Commun. 10, 4950 (2019).
Findley, K. et al. Phylogeny and phenotypic characterization of pathogenic Cryptococcus species and closely related saprobic taxa in the Tremellales. Eukaryot. Cell 8, 353–361 (2009).
White, T. C. et al. Fungi on the skin: dermatophytes and Malassezia. Cold Spring Harb. Perspect. Med. https://doi.org/10.1101/cshperspect.a019802 (2014).
Rodrigues, A. M. et al. The threat of emerging and re-emerging pathogenic Sporothrix species. Mycopathologia 185, 813–842 (2020).
Steenbergen, J. N., Shuman, H. A. & Casadevall, A. Cryptococcus neoformans interactions with amoebae suggest an explanation for its virulence and intracellular pathogenic strategy in macrophages. Proc. Natl Acad. Sci. USA 98, 15245–15250 (2001).
Casadevall, A., Fu, M. S., Guimaraes, A. J. & Albuquerque, P. The ‘Amoeboid Predator-Fungal Animal Virulence’ hypothesis. J. Fungi https://doi.org/10.3390/jof5010010 (2019).
Magditch, D. A., Liu, T. B., Xue, C. & Idnurm, A. DNA mutations mediate microevolution between host-adapted forms of the pathogenic fungus Cryptococcus neoformans. PLoS Pathog. 8, e1002936 (2012).
Fu, M. S. et al. Amoeba predation of Cryptococcus neoformans results in pleiotropic changes to traits associated with virulence. mBio https://doi.org/10.1128/mBio.00567-21 (2021).
Albuquerque, P. et al. A hidden battle in the dirt: soil amoebae interactions with Paracoccidioides spp. PLoS Negl. Trop. Dis. 13, e0007742 (2019).
Sil, A. & Andrianopoulos, A. Thermally dimorphic human fungal pathogens–polyphyletic pathogens with a convergent pathogenicity trait. Cold Spring Harb. Perspect. Med. 5, a019794 (2014).
Boyce, K. J. & Andrianopoulos, A. Fungal dimorphism: the switch from hyphae to yeast is a specialized morphogenetic adaptation allowing colonization of a host. FEMS Microbiol. Rev. 39, 797–811 (2015).
Strope, P. K. et al. The 100-genomes strains, an S. cerevisiae resource that illuminates its natural phenotypic and genotypic variation and emergence as an opportunistic pathogen. Genome Res. 25, 762–774 (2015).
Raffa, N. & Keller, N. P. A call to arms: mustering secondary metabolites for success and survival of an opportunistic pathogen. PLoS Pathog. 15, e1007606 (2019).
Munoz, J. F., McEwen, J. G., Clay, O. K. & Cuomo, C. A. Genome analysis reveals evolutionary mechanisms of adaptation in systemic dimorphic fungi. Sci. Rep. 8, 4473 (2018).
Mixao, V. & Gabaldon, T. Hybridization and emergence of virulence in opportunistic human yeast pathogens. Yeast 35, 5–20 (2018).
Maxwell, C. S. et al. Gene exchange between two divergent species of the fungal human pathogen, Coccidioides. Evolution 73, 42–58 (2019).
Gusa, A. et al. Transposon mobilization in the human fungal pathogen Cryptococcus is mutagenic during infection and promotes drug resistance in vitro. Proc. Natl Acad. Sci. USA 117, 9973–9980 (2020).
Bennett, R. J., Forche, A. & Berman, J. Rapid mechanisms for generating genome diversity: whole ploidy shifts, aneuploidy, and loss of heterozygosity. Cold Spring Harb. Perspect. Med. https://doi.org/10.1101/cshperspect.a019604 (2014).
Steenwyk, J. L., Soghigian, J. S., Perfect, J. R. & Gibbons, J. G. Copy number variation contributes to cryptic genetic variation in outbreak lineages of Cryptococcus gattii from the North American Pacific Northwest. BMC Genomics 17, 700 (2016).
Cisse, O. H. et al. Genomic insights into the host specific adaptation of the Pneumocystis genus. Commun. Biol. 4, 305 (2021).
Ianiri, G. et al. HGT in the human and skin commensal Malassezia: a bacterially derived flavohemoglobin is required for NO resistance and host interaction. Proc. Natl Acad. Sci. USA 117, 15884–15894 (2020).
Sun, S., Hoy, M. J. & Heitman, J. Fungal pathogens. Curr. Biol. 30, R1163–R1169 (2020).
Taylor, J. W. Evolutionary perspectives on human fungal pathogens. Cold Spring Harb. Perspect. Med. https://doi.org/10.1101/cshperspect.a019588 (2014).
Steenwyk, J. L. et al. Variation among biosynthetic gene clusters, secondary metabolite profiles, and cards of virulence across aspergillus species. Genetics 216, 481–497 (2020).
Jackson, A. P. et al. Comparative genomics of the fungal pathogens Candida dubliniensis and Candida albicans. Genome Res. 19, 2231–2244 (2009).
Carroll, S. B. Evolution at two levels: on genes and form. PLoS Biol. 3, e245 (2005).
Sorrells, T. R. & Johnson, A. D. Making sense of transcription networks. Cell 161, 714–723 (2015).
Fisher, K. J. & Lang, G. I. Experimental evolution in fungi: an untapped resource. Fungal Genet. Biol. 94, 88–94 (2016).
Forche, A. et al. Rapid phenotypic and genotypic diversification after exposure to the oral host niche in Candida albicans. Genetics 209, 725–741 (2018).
de Crecy, E., Jaronski, S., Lyons, B., Lyons, T. J. & Keyhani, N. O. Directed evolution of a filamentous fungus for thermotolerance. BMC Biotechnol. 9, 74 (2009).
Tso, G. H. W. et al. Experimental evolution of a fungal pathogen into a gut symbiont. Science 362, 589–595 (2018).
Hu, G. et al. Microevolution during serial mouse passage demonstrates FRE3 as a virulence adaptation gene in Cryptococcus neoformans. mBio 5, e00941–00914 (2014).
Ene, I. V. et al. Global analysis of mutations driving microevolution of a heterozygous diploid fungal pathogen. Proc. Natl Acad. Sci. USA 115, E8688–E8697 (2018).
Forche, A. et al. Selection of Candida albicans trisomy during oropharyngeal infection results in a commensal-like phenotype. PLoS Genet. 15, e1008137 (2019).
Lucking, R. et al. Fungal taxonomy and sequence-based nomenclature. Nat. Microbiol. 6, 540–548 (2021).
Cao, C., Xi, L. & Chaturvedi, V. Talaromycosis (Penicilliosis) due to Talaromyces (Penicillium) marneffei: insights into the clinical trends of a major fungal disease 60 years after the discovery of the pathogen. Mycopathologia 184, 709–720 (2019).
Fishman, J. A. Pneumocystis jiroveci. Semin. Respir. Crit. Care Med. 41, 141–157 (2020).
Gabaldon, T. & Carrete, L. The birth of a deadly yeast: tracing the evolutionary emergence of virulence traits in Candida glabrata. FEMS Yeast Res. 16, fov110 (2016).
Grigoriev, I. V. et al. MycoCosm portal: gearing up for 1,000 fungal genomes. Nucleic Acids Res. 42, D699–D704 (2014).
Shen, X. X. et al. Genome-scale phylogeny and contrasting modes of genome evolution in the fungal phylum Ascomycota. Sci. Adv. 6, eabd0079 (2020).
Shen, X. X. et al. Tempo and mode of genome evolution in the budding yeast subphylum. Cell 175, 1533–1545 (2018).
Robert, V. et al. MycoBank gearing up for new horizons. IMA Fungus 4, 371–379 (2013).
Nguyen, N. H. et al. FUNGuild: an open annotation tool for parsing fungal community datasets by ecological guild. Fungal Ecol. 20, 241–248 (2016).
Wang, F. et al. Transcription in fungal conidia before dormancy produces phenotypically variable conidia that maximize survival in different environments. Nat. Microbiol. 6, 1066–1081 (2021).
Zhao, S., Ge, W., Watanabe, A., Fortwendel, J. R. & Gibbons, J. G. Genome-wide association for itraconazole sensitivity in non-resistant clinical isolates of Aspergillus fumigatus. Front. Fung. Biol. 1, 617338 (2021).
Barber, A. E. et al. Aspergillus fumigatus pan-genome analysis identifies genetic variants associated with human infection. Nat. Microbiol. 6, 1526–1536 (2021).
Smith, S. D., Pennell, M. W., Dunn, C. W. & Edwards, S. V. Phylogenetics is the new genetics (for most of biodiversity). Trends Ecol. Evol. 35, 415–425 (2020).
Mazi, P. B., Rauseo, A. M. & Spec, A. Blastomycosis. Infect. Dis. Clin. North Am. 35, 515–530 (2021).
Pappas, P. G., Lionakis, M. S., Arendrup, M. C., Ostrosky-Zeichner, L. & Kullberg, B. J. Invasive candidiasis. Nat. Rev. Dis. Prim. 4, 18026 (2018).
Van Dyke, M. C. C., Thompson, G. R., Galgiani, J. N. & Barker, B. M. The rise of Coccidioides: forces against the dust devil unleashed. Front. Immunol. 10, 2188 (2019).
Maziarz, E. K. & Perfect, J. R. Cryptococcosis. Infect. Dis. Clin. North Am. 30, 179–206 (2016).
Schwartz, I. S. et al. Emergomyces: the global rise of new dimorphic fungal pathogens. PLoS Pathog. 15, e1007977 (2019).
Batista, B. G., Chaves, M. A., Reginatto, P., Saraiva, O. J. & Fuentefria, A. M. Human fusariosis: an emerging infection that is difficult to treat. Rev. Soc. Bras. Med. Trop. 53, e20200013 (2020).
Bahr, N. C., Antinori, S., Wheat, L. J. & Sarosi, G. A. Histoplasmosis infections worldwide: thinking outside of the Ohio River valley. Curr. Trop. Med. Rep. 2, 70–80 (2015).
Ruan, Y. et al. The largest meta-analysis on the global prevalence of microsporidia in mammals, avian and water provides insights into the epidemic features of these ubiquitous pathogens. Parasites Vectors 14, 186 (2021).
Prakash, H. & Chakrabarti, A. Global epidemiology of mucormycosis. J. Fungi https://doi.org/10.3390/jof5010026 (2019).
Martinez, R. New trends in paracoccidioidomycosis epidemiology. J. Fungi https://doi.org/10.3390/jof3010001 (2017).
Brown, L., Leck, A. K., Gichangi, M., Burton, M. J. & Denning, D. W. The global incidence and diagnosis of fungal keratitis. Lancet Infect. Dis. 21, e49–e57 (2021).
Plaignaud, M. Obervation sur un fongus du sinus maxillaire. J. de Chirugie 87, 244–251 (1791).
Knoke, M. & Bernhardt, H. The first description of an oesophageal candidosis by Bernhard von Langenbeck in 1839. Mycoses 49, 283–287 (2006).
Chander, J. Textbook of Medical Mycology 4th edn, 534–596 (Jaypee Brothers Medical Publishers Ltd., 2018).
Dawson, T. L. Jr Malassezia: the forbidden kingdom opens. Cell Host Microbe 25, 345–347 (2019).
Hirschmann, J. V. The early history of coccidioidomycosis: 1892–1945. Clin. Infect. Dis. 44, 1202–1207 (2007).
Bradsher, R. W.Jr The endemic mimic: blastomycosis an illness often misdiagnosed. Trans. Am. Clin. Climatol. Assoc. 125, 188–203 (2014).
Freij, J. B. & Freij, B. J. The earliest account of human cryptococcosis (Busse–Buschke Disease) in a woman with chronic osteomyelitis of the tibia. Pediatr. Infect. Dis. J. 34, 1278 (2015).
Lopes-Bezerra, L. M. et al. Sporotrichosis between 1898 and 2017: the evolution of knowledge on a changeable disease and on emerging etiological agents. Med. Mycol. 56, 126–143 (2018).
Benard, G. Pathogenesis and classification of paracocidioidomycosis: new insights from old good stuff. Open Forum Infect. Dis. 8, ofaa624 (2021).
Collins, R. D. Dr William DeMonbreun: description of his contributions to our understanding of histoplasmosis and analysis of the significance of his work. Hum. Pathol. 36, 453–464 (2005).
Walzer, P. D. The ecology of Pneumocystis: perspectives, personal recollections, and future research opportunities. J. Eukaryot. Microbiol. 60, 634–645 (2013).
Schneider, E. et al. A coccidioidomycosis outbreak following the Northridge, Calif, earthquake. JAMA 277, 904–908 (1997).
Gremiao, I. D., Miranda, L. H., Reis, E. G., Rodrigues, A. M. & Pereira, S. A. Zoonotic epidemic of sporotrichosis: cat to human transmission. PLoS Pathog. 13, e1006077 (2017).
Stephen, C., Lester, S., Black, W., Fyfe, M. & Raverty, S. Multispecies outbreak of cryptococcosis on southern Vancouver Island, British Columbia. Can. Vet. J. 43, 792–794 (2002).
Chang, D. C. et al. Multistate outbreak of Fusarium keratitis associated with use of a contact lens solution. JAMA 296, 953–963 (2006).
Neblett Fanfair, R. et al. Necrotizing cutaneous mucormycosis after a tornado in Joplin, Missouri, in 2011. N. Engl. J. Med. 367, 2214–2225 (2012).
Vaux, S. et al. Multicenter outbreak of infections by Saprochaete clavata, an unrecognized opportunistic fungal pathogen. mBio https://doi.org/10.1128/mBio.02309-14 (2014).
Larone, D. H. & Walsh, T. J. Exserohilum rostratum: anatomy of a national outbreak of fungal meningitis. Clin. Microbiol. Newsl. 35, 185–193 (2013).
Hoenigl, M. Invasive fungal disease complicating Coronavirus disease 2019: when it rains, it spores. Clin. Infect. Dis. 73, e1645–e1648 (2021).
Hubka, V. et al. Unravelling species boundaries in the Aspergillus viridinutans complex (section Fumigati): opportunistic human and animal pathogens capable of interspecific hybridization. Persoonia 41, 142–174 (2018).
Knowles, S. L. et al. Mapping the fungal battlefield: using in situ chemistry and deletion mutants to monitor interspecific chemical interactions between fungi. Front. Microbiol. 10, 285 (2019).
Oberlies, N. H. et al. Droplet probe: coupling chromatography to the in situ evaluation of the chemistry of nature. Nat. Prod. Rep. 36, 944–959 (2019).
Lamoth, F. Aspergillus fumigatus-related species in clinical practice. Front. Microbiol. 7, 683 (2016).
Cox, M. J., Loman, N., Bogaert, D. & O’Grady, J. Co-infections: potentially lethal and unexplored in COVID-19. Lancet Microbe 1, e11 (2020).
Crum-Cianflone, N. F. Invasive aspergillosis associated with severe influenza infections. Open Forum Infect. Dis. 3, ofw171 (2016).
Ezeokoli, O. T., Gcilitshana, O. & Pohl, C. H. Risk factors for fungal co-infections in critically ill COVID-19 patients, with a focus on immunosuppressants. J. Fungi https://doi.org/10.3390/jof7070545 (2021).
Koehler, P. et al. COVID-19 associated pulmonary aspergillosis. Mycoses 63, 528–534 (2020).
Alanio, A., Delliere, S., Fodil, S., Bretagne, S. & Megarbane, B. Prevalence of putative invasive pulmonary aspergillosis in critically ill patients with COVID-19. Lancet Respir. Med. 8, e48–e49 (2020).
Prattes, J. et al. Diagnosis and treatment of COVID-19 associated pulmonary apergillosis in critically ill patients: results from a European confederation of medical mycology registry. Intensive Care Med. https://doi.org/10.1007/s00134-021-06471-6 (2021).
Arastehfar, A. et al. COVID-19 associated pulmonary aspergillosis (CAPA)—from immunology to treatment. J. Fungi https://doi.org/10.3390/jof6020091 (2020).
John, T. M., Jacob, C. N. & Kontoyiannis, D. P. When uncontrolled diabetes mellitus and severe COVID-19 converge: the perfect storm for mucormycosis. J. Fungi 7, 298 (2021).
Steenwyk, J. L. et al. Genomic and phenotypic analysis of COVID-19-associated pulmonary aspergillosis isolates of Aspergillus fumigatus. Microbiol. Spectr. https://doi.org/10.1128/Spectrum.00010-21 (2021).
Casadevall, A. The pathogenic potential of a microbe. mSphere https://doi.org/10.1128/mSphere.00015-17 (2017).
Keizer, E. M. et al. Variation of virulence of five Aspergillus fumigatus isolates in four different infection models. PLoS ONE 16, e0252948 (2021).
Cramer, R. A. & Kowalski, C. H. Is it time to kill the survival curve? A case for disease progression factors in microbial pathogenesis and host defense research. mBio https://doi.org/10.1128/mBio.03483-20 (2021).
Garcia-Solache, M. A. & Casadevall, A. Global warming will bring new fungal diseases for mammals. mBio 1, e00061-10 (2010).
Nnadi, N. E. & Carter, D. A. Climate change and the emergence of fungal pathogens. PLoS Pathog. 17, e1009503 (2021).
Rhodes, J. & Fisher, M. C. Global epidemiology of emerging Candida auris. Curr. Opin. Microbiol. 52, 84–89 (2019).
Chow, N. A. et al. Tracing the evolutionary history and global expansion of Candida auris using population genomic analyses. mBio 11, e03364-19 (2020).
Lockhart, S. R. et al. Simultaneous emergence of multidrug-resistant Candida auris on 3 continents confirmed by whole-genome sequencing and epidemiological analyses. Clin. Infect. Dis. 64, 134–140 (2017).
Casadevall, A., Kontoyiannis, D. P. & Robert, V. Environmental Candida auris and the global warming emergence hypothesis. mBio https://doi.org/10.1128/mBio.00360-21 (2021).
Arora, P. et al. Environmental isolation of Candida auris from the Coastal Wetlands of Andaman Islands, India. mBio https://doi.org/10.1128/mBio.03181-20 (2021).
Taylor, J. W. et al. Sources of fungal genetic variation and associating it with phenotypic diversity. Microbiol Spectr. https://doi.org/10.1128/microbiolspec.FUNK-0057-2016 (2017).
Kim, N.-S. The genomes and transposable elements in plants: are they friends or foes? Gene. Genom. 39, 359–370 (2017).
Cortés-Ortiz, L., Roos, C. & Zinner, D. Introduction to special issue on primate hybridization and hybrid zones. Int. J. Primatol. 40, 1–8 (2019).
Gogarten, J. P. & Townsend, J. P. Horizontal gene transfer, genome innovation and evolution. Nat. Rev. Microbiol. 3, 679–687 (2005).
Shastry, B. S. SNPs in disease gene mapping, medicinal drug development and evolution. J. Hum. Genet. 52, 871–880 (2007).
Powell, R. V., Willett, C. R., Goertzen, L. R. & Rashotte, A. M. Lineage specific conservation of cis-regulatory elements in Cytokinin Response Factors. Sci. Rep. 9, 13387 (2019).
Campbell, M. A., Buser, T. J., Alfaro, M. E. & López, J. A. Addressing incomplete lineage sorting and paralogy in the inference of uncertain salmonid phylogenetic relationships. PeerJ 8, e9389 (2020).
Acknowledgements
I thank past and present members of my laboratory, in particular M. Mead and J. Steenwyk, and my collaborators C. T. Hittinger, G. Goldman and N. Oberlies for numerous discussions over the years that have shaped my thinking on the topic. I thank Y. Li for his help with Fig. 1. Research in my laboratory is supported by the National Institutes of Health/National Institute of Allergy and Infectious Diseases (grant nos R56 AI146096 and R01 AI153356), National Science Foundation (grant nos DEB1442113 and DEB2110404), Guggenheim Foundation and Burroughs Wellcome Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
I am a scientific consultant for LifeMine Therapeutics, Inc.
Peer review
Peer review information
Nature Microbiology thanks Daniel Croll and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Fig. 1.
Rights and permissions
About this article
Cite this article
Rokas, A. Evolution of the human pathogenic lifestyle in fungi. Nat Microbiol 7, 607–619 (2022). https://doi.org/10.1038/s41564-022-01112-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41564-022-01112-0
This article is cited by
-
Plastiphily is linked to generic virulence traits of important human pathogenic fungi
Communications Earth & Environment (2024)
-
Streptomyces griseus Versus Trichoderma viride Chitinase as an Anti-inflammatory and Antifungal Agent Against Human Pathogenic Fungi
Indian Journal of Microbiology (2024)
-
Development of a chitosan derivative bearing the thiadiazole moiety and evaluation of its antifungal and larvicidal efficacy
Polymer Bulletin (2024)
-
Exploring therapeutic avenues: mesenchymal stem/stromal cells and exosomes in confronting enigmatic biofilm-producing fungi
Archives of Microbiology (2024)
-
The Impact of Climate Change on Human Fungal Pathogen Distribution and Disease Incidence
Current Clinical Microbiology Reports (2024)