Universal health coverage (UHC) is what the world is working toward. It’s a future state where everyone everywhere has fair access to the basic health products and services required to live a healthy life. Primary health care (PHC) is the system of services that can make UHC a reality.
In contrast to historically siloed health services focused on treating sick people or providing standard preventive interventions such as childhood immunizations, holistic PHC systems aim to keep people healthy by providing a complete package of health promotion and disease prevention, treatment, rehabilitation, and palliation services. Throughout a person’s lifetime, 80 percent of the health services they receive will be delivered through a PHC system.
To accelerate global progress toward UHC, PATH and our partners are supporting governments and health departments in five key ways:
1. Increasing health system resilience
A health system’s ability to identify and respond to emerging health threats is central to its resilience. Since the emergence of COVID-19, PATH has been partnering with countries to adapt and transform their pandemic response measures into sustainable national, subnational, and local interventions like community-based surveillance, diagnostic networks, and vaccine administration mechanisms.
Once established, these tools and mechanisms increase health system resilience by making it easier to identify and respond to future epidemics, easier to maintain essential health services during epidemics or other disruptions, and easier to track and mitigate antimicrobial resistance (AMR), effects from climate change, and other emerging barriers to health equity.
“By uniting two historically siloed efforts—PHC and epidemic preparedness and response—we can increase health system resilience by ensuring outbreaks, AMR, and patient-centered care can be managed by existing health infrastructure. This involves building flexible, scalable systems for diagnosis, clinical care, and oversight,” says Dr. Linda Venczel, Director of the Epidemic Preparedness and Response program at PATH. “For example, in Vietnam we have worked during the pandemic to develop self-testing for COVID-19 and an electronic vaccine passport system that protects the individual and helps emergency preparedness and response teams track areas with low coverage and where surveillance needs to be supplemented.”
In Malawi, oxygen demand created by COVID-19 pushed the country’s medical oxygen systems beyond capacity. PATH partnered with the Ministry of Health and UNICEF, and together we developed Malawi’s first national medical oxygen roadmap—a structured and attainable plan to establish and maintain the collective of people, processes, equipment, and logistics that are required to deliver oxygen to a patient, beyond COVID-19 response. In India, we supported more than 125,000 facilities with planning, sourcing, and installing oxygen concentrators for COVID-19 patients. And in Vietnam, we worked with the Ministry of Health to identify and address gaps in medical oxygen access and respiratory care.
2. Investing in subnational health systems
PHC has long been recognized as the means of achieving UHC, but investments have fallen short or been too siloed to strengthen systems holistically. To make new progress toward global goals, governments and funders should invest not only in PHC—but in PHC systems—without taking resources away from essential health services, such as maternity care.
PATH supports governments and funders in the prioritization of national and subnational PHC investments, and in the development and passage of national policies and guidelines that enable the delivery of health services that reflect community needs.
The real-time data that these services and systems provide to health officials improves subnational leadership and decision-making on resource utilization, human resources for health, supply chains for family planning, reliable access to oxygen as part of a comprehensive respiratory care treatment package, contraceptive self-care, HIV self-testing kits, health insurance coverage, and overall health indices and outcomes.
“In India, Kenya, Senegal, and Tanzania, we are working in 305 PHC facilities to increase access to pulse oximetry and electronic clinical decision support algorithms. These tools allow health care workers to better detect severe illness through digital technologies,” says Mike Ruffo, Project Director, Tools for Integrated Management of Childhood Illness, PATH. “We’ve worked closely with leadership at the district level to design and implement these tools in a way that is consistent with current practices. This includes investing in health care worker training, supportive supervision, and monitoring and evaluation systems.”
3. Digitalizing health systems
The digital transformation of national health systems supports countries to overcome fundamental health system limitations that prevent effective diagnosis, treatment, and care for diseases that affect thousands of their citizens. The greater insights and capabilities offered by stronger digital and data systems enable policymakers and providers to target precious health care budgets and services for highest impact.
PATH partners closely with country stakeholders to strengthen the essential systems and technologies that equip people, providers, and governments with the data they need to make informed choices that improve health and save lives. For example, in Zambia, PATH partnered with Tableau and national health officials to design an approach that provides real-time analytics on malaria cases and available health services, making intervention coordination more effective and efficient. This use of data has led to substantially fewer malaria-related deaths, with a 90 percent decline in Zambia’s Southern Province. In Vietnam, PATH and Tableau helped the country build an emergency operations center that uses the same methodology to monitor a variety of communicable diseases.
Digital transformation supports health services beyond the data needed for better care by ensuring consistent availability of the essential resources needed for care. Our partnerships with the ministries of health in Kenya and Uganda led to development of a tool to forecast the essential products needed to manage noncommunicable diseases, which in turn led to five-year procurement forecasts for hypertension and diabetes medicines for the first time ever. The result will be more strategic financing and procurement of these medicines and greater availability throughout public health supply chains.
Meanwhile, the COVID-19 pandemic has greatly accelerated digital development. Where once PATH looked at how digital transformation could address global health issues, with COVID-19, a health issue has accelerated the global digital transformation. In the DRC, PATH supported the government to rapidly establish a national COVID-19 digital data collection, integration, and analysis system that allows the government to coordinate its pandemic response. In India, we found ways to simplify COVID-19 data entry with a single point tool to translate response efforts into long-term improvements in health systems across the country. Again in India and also in Kenya, Ukraine, and Vietnam, we supported the expansion of virtual patient care in response to COVID-19. These measures, if sustained, will ensure community-preferred options that over time will contribute to greater access, quality, and affordability of health services.
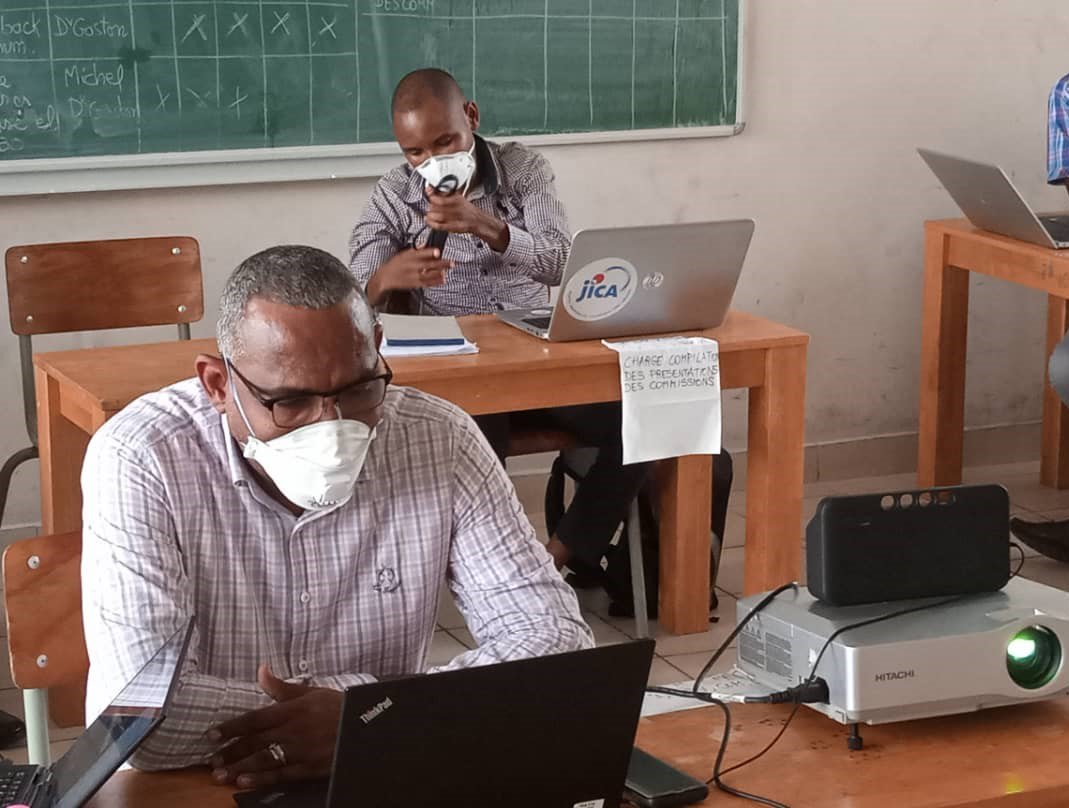
In the Democratic Republic of the Congo (DRC), members of the COVID-19 task force train on digital tools to stay connected during the pandemic. Photo: PATH/Trad Hatton.
These technologies and approaches are not a panacea. In combination with strong leadership and capacity strengthening, however, they are powerful contributors toward solving systemic problems that inhibit progress toward UHC.
4. Prioritizing self-care
The World Health Organization defines self-care as “the ability of individuals, families and communities to promote health, prevent disease, maintain health, and cope with illness and disability with or without the support of a healthcare provider.”
Supporting self-care makes the best use of domestic funding for health, leads to new and sometimes breakthrough health care approaches, and improves access to medicines. To this end, PATH works with private-sector providers such as pharmacies, clinics, and e-commerce to expand access to innovative self-care products, including self-testing options for HIV, TB, viral hepatitis, sexually transmitted infections, family planning, mental health, diabetes, hypertension, COVID-19, and some cancers.
With expanded testing options that are convenient and confidential, individuals and communities have fast, easy access to treatment and management of chronic conditions like hypertension or infectious diseases like TB. And by taking pressure off overburdened clinics, these self-care innovations enable countries to maintain essential services as national systems manage the COVID-19 pandemic.

Dr. Ali Kitoko shares information on an HIV self-test at Pharmacie Binamet in Haut-Katanga Province, Democratic Republic of the Congo, to introduce pharmacist-assisted HIV self-testing services during COVID-19. Photo: PATH/Raphael Mwamba.
5. Focusing on people-centered care
People-centered care incorporates the desires and needs of individuals and communities into the design of health infrastructure and services. PATH uses tools like behavioral science and human-centered design to identify barriers to care and co-create solutions with users. This results in health products, policies, and systems that are more inclusive and of a higher quality than those currently available. To advance equity, PATH engages diverse stakeholders, including adolescents and youth, in the design of innovations that work for them.
“Through close collaboration with ministries of health and other local partners, PATH has helped to integrate care, offer preventative screenings in easier-to-reach places, and develop usable, person-centered interventions in countries all over the world,” says Dr. Kimberly Green, PATH’s Director of Primary Health Care. “These approaches have shown improved health outcomes, more targeted investments, and more resilient health systems.”
In India, PATH and Access Accelerated recently conducted a landscape assessment to gain a better understanding of the barriers and facilitators to care for noncommunicable diseases and to develop priority investment areas for more accessible, higher-quality care. In Vietnam, we partnered with a local grocery store chain so people can shop for groceries and get screened for hypertension and diabetes all in one place, bringing health care services closer to people’s everyday lives. Also in Vietnam, we have integrated mental health with HIV services for people at dual risk.

Community volunteers screen a Co.opMart customer for hypertension (photo taken before Vietnam's January 2021 COVID-19 wave). Photo: PATH/Hung Nguyen Manh.
Across geographies, we put our expertise in sexual and reproductive health to use by developing products that meet the needs of women and girls, increasing access to cervical cancer screening and treatment, and creating new technologies for HIV and pregnancy prevention. In seven countries, the PATH-JSI DMPA-SC Access Collaborative has supported policies that advance access to DPMA-SC, a new self-injectable contraceptive option, as part of a broad range of voluntary family planning methods.
A healthier world is possible
We cannot relent in our focus on health for all. COVID-19 has taught us that addressing pandemics, epidemics, and other persistent health challenges requires unity and investment. To achieve UHC, we must keep PHC at the top of global, national, and subnational agendas, and work to address broader determinants of health. PATH, peer nongovernmental organizations, governments, and communities must work together to build systems that keep people at the center.



