-
PDF
- Split View
-
Views
-
Cite
Cite
Monica Schoch-Spana, An Epidemic Recovery Framework to Jump-start Analysis, Planning, and Action on a Neglected Aspect of Global Health Security, Clinical Infectious Diseases, Volume 71, Issue 9, 1 November 2020, Pages 2516–2520, https://doi.org/10.1093/cid/ciaa486
Close - Share Icon Share
Abstract
Epidemic readiness and response command the disproportionate attention of health security decision makers, planners, and practitioners, overshadowing recovery. How patients and their families, health organizations, community sectors, and entire societies recuperate from major outbreaks requires more systematic study and better translation into policy and guidance. To help remedy this neglected aspect of health emergency management, we offer a working definition for epidemic recovery and a preliminary model of postepidemic recovery. Guiding this framework’s development are insights gleaned from the more mature study of postdisaster reconstruction and rehabilitation as well as recognition that postoutbreak recovery—which involves infectious disease, a biological hazard—presents challenges and opportunities distinct from events involving geological or meteorological hazards. Future work includes developing a consensus around characteristics of successful epidemic recovery, applying these metrics to support preincident planning for postepidemic recovery, and using such a scheme to track and inform actual recovery from an epidemic.
In its first annual report (issued September 2019), the Global Preparedness Monitoring Board (GPMB) warned of “a new era of high-impact, potentially fast-spreading outbreaks that are more frequently detected and increasingly difficult to manage” [1], noting that the World Health Organization (WHO) tracked 1483 epidemic events in 172 countries between 2011 and 2018. With infectious disease threats, as well as their social, economic, and political impacts growing, the international public health community and national governments have stepped up efforts over the last 15 years to avert outbreaks and their potential escalation into transnational emergencies. Critical to this aim have been the 2005 International Health Regulations, the governing framework for global health security [2], and the Joint External Evaluation Tool through which countries can assess and track their capacity to prevent, detect, and rapidly respond to public health threats [3].
These 2 foundational works—which have helped advance outbreak readiness and response worldwide—nonetheless scarcely address the process of outbreak recovery. The period of postepidemic rehabilitation continues to be an analytic and practical gap according to the EcoHealth Alliance’s 2019 review of the major global health security initiatives now under way, including ones prompted by the 2014 West Africa Ebola outbreak [4]. Confirming this assessment is a WHO evaluation in 2019 of high-level recommendations focused upon national preparedness and health emergency management [5]. By contrast, the international doctrine evolving originally out of a natural disaster focus (vs a public health and infectious disease focus) specifies recovery in detail as part of a larger risk management strategy [6]. One Health guidance on risk at the human-animal-environment interface, too, similarly problematizes recovery [7].
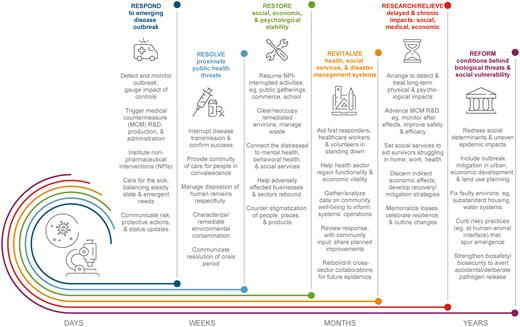
To advance global health security’s treatment of recovery as a pressing concern, on par with readiness and response, this commentary provides a working definition and calls for more analysis, planning, and action at a level commensurate with the issue’s importance to affected individuals and communities. Major learnings from the more mature study of disaster recovery are also reviewed to help hasten development of an organizing framework for postepidemic recuperation. Closing with a model of postepidemic recovery (Figure 1), the commentary invites experts to engage with the construct’s underlying assumptions as a way to help refine our collective thinking on what signifies and enables overall healing—at both the individual and population health level—after infectious disease strikes.
Epidemic recovery: processes and sample steps. Abbreviations: MCM, medical countermeasure; NPI, nonpharmaceutical intervention; R&D, research and development.
As of this writing, the coronavirus disease 2019 (COVID-19) pandemic continues to unfold, with scattered disease hotspots and as-yet untouched areas. The emergency response is still in full force. Nonetheless, the discussion provided here may assist communities in envisioning what outcomes signify that they have transitioned from a state of crisis to one of repair and regeneration, as well as improved preparation for the next infectious disease emergency.
DEFINING EPIDEMIC RECOVERY
In its mainstream formulation, epidemic management has an urgent but narrow focus: containing the spread of disease and caring for the sick and dying. As the tail end of an epidemiological curve trails off, many people assume that the concerning public health event is somehow over and that a return to business as usual is under way [8, 9]. The lived experiences of affected communities, organizations, and individuals, however, suggest otherwise.
Survivors May Have Lingering Medical Conditions, Financial Burdens, Emotional Support Needs, and Social Service Requirements
In the case of a Zika virus outbreak, recovery can be long and complex: Guillain-Barré syndrome can diminish productivity and household budgets, pregnancy loss can prompt complicated grieving and need for moral support, and congenital Zika syndrome can mean ongoing medical and social service needs for affected children [10]. Enduring impacts of an infectious agent can take several forms, all with reverberating social and economic impacts: ongoing damage due to persistent infection or immune response (eg, Chikungunya virus–induced chronic inflammatory rheumatism), lifelong disability due to the initial acute infection (eg, poliovirus-induced permanent paralysis), and indirect vulnerabilities (eg, measles virus–induced preterm birth and neurological deficits) [11].
Healthcare facilities may struggle to regain full functionality due to workforce depletion, revenue losses, stigmatization, and/or contamination. Due to its rapid nosocomial transmission, severe acute respiratory syndrome (SARS) sickened healthcare workers disproportionately, prompted posttraumatic stress disorder through severe emotional distress, and contributed to employee burnout and low productivity. Moreover, SARS affected hospitals’ revenues due to decreased healthcare utilization and medical services [12, 13]. During the 2014 Ebola outbreak, the facility that admitted the imported index case of Ebola in Nigeria had key staff members perish of the disease, saw employees and the institution stigmatized, and lost significant market share, revenue, and brand equity [14].
Communities may require extra efforts to revitalize commerce, repair social schisms, recoup trust in government, and reconfigure health and human services delivery. Fear during the West African Ebola outbreak led to stigma, lost faith in health services, and social fracturing. Communities have had to reconfigure social roles due to lost parents, wage earners, teachers, and local leaders, and to restore the rhythm of activity for schools, public services, industry, markets, agriculture, and the health sector [15]. Communities severely affected by Zika confront the need to aid families of children with microcephaly; having to assume added childcare duties, women are at disproportionate risk of permanently leaving the workforce and losing income and the autonomy it confers [10].
Improving our understanding of, as well as support for households, organizations, sectors, and whole communities as they rebound postepidemic requires a much longer and broader view on outbreak management than a crisis response mindset permits. Disaster recovery analysts have carefully delineated their object of concern [16, 17]. Following their lead and recognizing the complex human experience with infectious disease, we define epidemic recovery as the following: “the decisions and actions, both planned before and improvised after a major outbreak, that enable the restoration, revitalization, and reformation of the social, economic, physical, and natural systems impinging upon human health and well-being.”
LEARNING FROM DISASTER RECOVERY RESEARCH
Reviewing studies of postdisaster rehabilitation/restoration more closely—that is, absorbing their lessons and avoiding their missteps—can help accelerate the development of a framework to guide epidemic recovery research, strategy, and operations. The principles below represent key learnings that can help inform future constructs of postoutbreak healing.
Think Holistically, Broadening the Focus Beyond the Immediately Discernible Damages
Early disaster research erred in equating recovery with reconstruction of the physical environment—clearing debris, getting infrastructure back online, rebuilding housing and commercial facilities, and so on [18–20]. Only later was importance given to social, emotional, economic, political, and natural realms. Beyond material reconstruction is the reconstitution of a sense of safety, social connections, faith in institutions, and economic exchange. Theories of epidemic recovery, too, should avoid an analogous equation of recovery with the obvious yet still narrow indicators of interrupted disease transmission, clinically resolved infections, and a functional health sector. Such a caution is helpful, because the emerging emphasis within global health security regarding the postepidemic context is, understandably, health sector reconstitution and strengthening [21].
Anticipate Messiness, Seeing Recovery as a Complex, Nonlinear, Unevenly Achieved Process
At its outset, disaster recovery scholarship generated “phased” models with predicted timelines and uniform progression [22]. Yet, further inquiry revealed a process that unfolded in fits and starts, proceeding unevenly across populations and critical community functions and with “fuzzy” endpoints. Now, disaster researchers acknowledge that so-called recovery stages overlap with one another; that actions taken during response influence recovery trajectories; and that preexisting vulnerabilities and capabilities affect if, how, and when different social groups achieve recovery milestones [20]. We, too, should avoid models of epidemic recovery that reinforce notions of a process unfolding in neat, preordained phases. In an epidemic, for instance, the uncertainties during the response—for example, whether a safe and effective medical countermeasure (MCM) exists, the MCM supply and operational capacity for its mass distribution are sufficient, and people of all backgrounds trust in the authorities who recommend taking the MCM [23]—can strongly influence the nature and enormity of the recovery.
Specify the Unit of Analysis, Knowing the Differential Nature of Recovery Processes and Outcomes
Not presuming steady progression toward a singular postdisaster state of well-being, researchers grasp recovery as a multilevel process. The unit of analysis matters, for example, nation, region, community, sector, organization, neighborhood, or household [18–20]. While an entire community is seemingly back to normal after an earthquake or hurricane, the number and quality of critical services may still lag in certain neighborhoods. Response and recovery organizations may judge rehabilitation as complete according to community-scale metrics, yet a disaster’s financial and emotional effects may still linger for individual households and persons. In the case of an epidemic, also, the focal point or points for observing recovery processes and outcomes are important. Analyses of the 2009 H1N1 influenza pandemic confirm racial and ethnic disparities in morbidity, hospitalization, and mortality that were driven by sociocultural and economic factors; these effects augur a more difficult recovery for specific social groups than that revealed by undifferentiated health data at the whole population level [24].
Recognize that Event Severity and Scope Influence the Pace and Quality of Recovery
Disaster recovery researchers envision a continuum of challenges—increasing in gravity and complexity—associated with event magnitude: for example, stretching from a small-scale event such as an F2 tornado of limited length, to a moderate disaster such as flash flooding to < 5 feet, to a catastrophe producing massive damage, such as Hurricane Katrina [25]. Truly catastrophic events present unique recovery difficulties in that their rarer occurrence leads to few opportunities for adaptive learning on the most effective ways to rebound from cataclysmic disaster effects [20]. Repetitive disaster losses also constitute a distinctive predicament for recovery, given the constant drain on community reserves. Similarly, the case of Ebola in West Africa speaks to the extraordinary hurdles of recovering from a totalizing epidemic in the context of chronic health challenges such as human immunodeficiency virus/AIDS, tuberculosis, and malaria as well as their broader societal effects [26]. The grave, lingering, and far-reaching impacts anticipated with a severe influenza pandemic [27], and experienced with the West African Ebola outbreak [15], have been among the few threat scenarios to have drawn attention to the challenges of postepidemic recovery.
Treat Recovery as Restoration, but to a “New Normal”—the Outlines of Which Are Potentially Subject to Volatile Debate
Competing impulses, aims, and interests characterize the postdisaster recovery period. Studies reveal, on one hand, a strong urge to return quickly to the status quo that may comfort in its familiarity but constitute proven vulnerability to disaster (eg, rebuilding in a floodplain), and on the other, a desire to “build back better,” resulting in greater disaster resilience and a better quality of life overall (eg, turning formerly developed floodplains into green space and building more stocks of affordable housing) [16, 18, 28]. Further complicating the pull between a known past and a hopeful future are power struggles over if and how the “new normal” may benefit some people over others [20]. The postepidemic context, too, can exhibit the potential for conflicts over how best to move forward. Inadequate health infrastructure as well as rifts between political leaders and populations exacerbated the Ebola epidemic in Liberia, Guinea, and Sierra Leone, and point to the need for fundamental reforms [9, 15].
MODELING POSTEPIDEMIC RECOVERY
To spark further analysis and action, we offer a preliminary model (Figure 1) depicting the processes of postepidemic recovery. We encourage researchers, policy makers, planners, and other professionals in global health security to consider whether and how the construct appropriately captures the theory and practice of recuperating from a major infectious disease emergency and which aspects warrant changes and further explication. In building the model, we have relied upon a range of source materials in public health, each of which holds a piece of the larger whole represented here, and upon our subject matter expertise in the areas of disaster recovery, community resilience, and emergency management.
In framing epidemic recovery, we applied the above-mentioned principles derived from disaster recovery studies. With the community as its unit of analysis, the model attends to the larger social, economic, physical, and natural systems that impinge upon human health and well-being, including support services, economic prospects, and crisis communications that help foster the recovery of affected groups and individuals according to a “whole person” model [29]. The model also treats recovery as both a process of restoration (eg, getting people well and on their feet; making the health sector fully functional again; curbing the stigmatization of people, places, and products) and transformation (eg, addressing the social determinants of uneven epidemic impacts; integrating resilience to epidemics into long-range planning not typically tied to health outcomes) [16, 28]. Last, the timeframe and activities of recovery are represented in a fluid manner, with different phases and functions overlapping and building up along a temporal continuum, from the early days of the acute response to the later years of fundamental reforms. In an actual epidemic, discontinuities in the progression of recovery are inevitable; nonetheless, the roughly logical sequence may be beneficial for planning purposes and model clarification.
While benefiting from the extant natural disaster literature, the model also recognizes that infectious diseases are biological hazards, and therefore, outbreaks present recovery challenges and opportunities distinct from events involving geological or meteorological hazards—for example, decontamination efforts to remove and/or render pathogens nonviable [30]; enhanced MCM research, development, and production to prevent and treat future infection [23]; heightened vulnerability of the health sector to outbreak impacts [12, 13]; potential secondary chronic health conditions and their socioeconomic effects that require longer-term support and intervention [11]; primary prevention and mitigation in the form of fewer risky practices at the human-animal-environment interface that lead to pathogen emergence [7]; and heightened biosecurity and biosafety measures to offset the risk of accidental or deliberate release of a dangerous pathogen [3].
Finally, as our experience and the bulk of our sources reflect a vantage from the United States, we invite colleagues from abroad to engage with the framework to examine its applicability and relevance in low- and middle-income countries. The lingering hold of the Ebola epidemic in the Democratic Republic of Congo (as of this writing), for instance, defies simple rendering of an outbreak’s immediate response and initial resolution, even more so the complex process of reforming a politically, economically, and ecologically fragile region into a more resilient one [31]. Future conceptualizations of epidemic recovery processes should provide a meaningful way to apprehend and convey postoutbreak strategies that appear to work in specific national and community settings.
Conclusions
At present, the response and readiness phases of epidemics capture the disproportionate notice of decision makers, planners, practitioners, and news sources. The process by which patients and their families, health organizations, community sectors, and whole societies recuperate from a severe outbreak requires more systematic study, better characterization, and translation into policy and guidance. By defining and modeling epidemic recovery, this commentary takes an important first step to help remedy a neglected aspect of global health security. As signaled by parallel advancements in disaster recovery research, key subsequent moves are obtaining agreement on the characteristics of successful epidemic recovery, applying such metrics in support of proactive epidemic recovery planning, and developing assessment tools with which to track the progress in a community’s recovery from epidemics [32].
Notes
Presented in part: Global Health Security 2019 Conference, Sydney, Australia, 18–20 June 2019.
Financial support. This work was supported by the Johns Hopkins Center for Health Security.
Potential conflicts of interest. The author has served as a consultant to J&M Global Solutions and reports grants from Open Philanthropy Project. The author has submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.




Comments